Congenital Diaphragmatic Hernia
- What is congenital diaphragmatic hernia?
- How is CDH diagnosed?
- What tests will be done?
- Possible pregnancy complications
- How does CDH affect my baby?
- How do you treat CDH?
- Stabilizing procedures
- Complications and therapies
- Pulmonary hypertension
- When will surgery be done?
- What happens after surgery?
- Will I be able to help care for my baby?
- When can my baby go home?
- What is my baby’s long-term prognosis?
What is congenital diaphragmatic hernia?
Congenital diaphragmatic hernia (CDH) is a hole in the muscle that separates the chest from the stomach area. This muscle is called the diaphragm. The cause of CDH is not known. It is not due to anything the mother ate or did while she was pregnant.
Because of this hole, some organs that should stay in the abdomen are up in the chest. This may include the stomach and intestine. This can cause severe problems.
If these organs are up in chest, the lungs may not grow as they should. This is because of the smaller space in the chest. The lungs may be underdeveloped (hypoplastic). Even though the defect is only on one side, CDH can affect both lungs.
Sometimes, the heart can be pushed out of its normal position. This shift may also reduce the amount of space for the lung on the other side
Many newborns with CDH will also have problems with other parts of their body.
How is CDH diagnosed?
It may be diagnosed during a routine ultrasound test. The test may show that heart shifted to the opposite side of the chest. It may also show that there are parts of the bowel in the chest.
Ifyour doctor suspects CDH, you will be referred to a doctor who handles high-risk pregnancies. This doctor is called a Maternal-Fetal Medicine Specialist. That doctor may do other tests to confirm the diagnosis or to get information about the baby’s outlook for you before delivery.
What tests will be done?
Your baby will be watched closely as the pregnancy goes on. You will most likely have many tests. These may include:
Ultrasound. This test may need to be done every 2 to 4 weeks. It looks at your baby’s growth and amount of amniotic fluid.
Amniocentesis with chromosomal analysis. This test is done to look for chromosome defects.
Fetal echocardiogram. This test is done to see if there are heart problems.
Fetal movement counting. This starts at about the 26th week of pregnancy. You will count your baby's movements once a day, for up to 2 hours. Your baby should move at least 10 times in 2 hours. If your baby moves 10 times in 2 hours or less, you are done counting for that day. If your baby is not moving, call your doctor right away.
Non-stress tests. You may begin to have non stress tests at about 32 weeks. These tests will be done 2 times each week.
Biophysical profile (BPP).
A BPP is an ultrasound study that checks:
- Amount of amniotic fluid.
- Your baby’s breathing movements.
- Movements of the arms and legs along with non-stress test results.
Fetal magnetic resonance imaging study (MRI). The MRI may give better information about the CDH. This may help you know what to expect when your baby is born. It does not use any radiation, so it is safe for both you and your baby.
Possible pregnancy complications
Some women will have more amniotic fluid than normal. This is called polyhydramnios. It puts the mother at risk for early (premature) labor and delivery. Early delivery puts the baby at risk for health issues. The lungs are one of the last organs to mature, so a baby born early will have lungs that are not fully mature.
How does CDH affect my baby?
At birth, the CDH can have serious effects on your baby’s ability to breathe. Your baby’s blood circulation may be affected by:
- Pressure in the chest and shifting of the heart.
- Abnormal development of the lungs and their blood vessels.
The size of the diaphragmatic hernia tells how much the lungs are affected. The prenatal ultrasound and fetal MRI may help tell how severe your baby’s condition will be.
How do you treat CDH?
Your baby will be checked right away after delivery. You will be able to see your baby. If possible, you will be able to hold your baby.
At birth, most babies with CDH need help to breathe. A tube will be put in your baby’s mouth to help with breathing. This tube passes through the vocal cords. While the tube is in, your baby will not be able to make sounds.
Another tube will be passed through your baby’s mouth and into the stomach. This keeps the stomach small so it does not press more on the lungs.
Stabilizing procedures
Most often, the umbilical cord has two arteries and a vein. A tube called an umbilical venous catheter (UVC) will be put in the vein in your baby’s umbilical cord. Vitamins, minerals, calories, fat and medicine can be given through this tube for a long time.
An arterial line called an umbilical artery catheter (UAC) will be put in one of the arteries of the umbilical cord. This line is used to give IV fluid, take blood for testing, and watch blood pressure.
Your baby may need some medicines before surgery. They include:
- Narcotics. These keep your baby free from pain.
- Paralytics. These keep your baby from moving.
- Blood pressure medicine may be needed to keep your baby’s blood pressure at a safe level.
Complications and therapies
There may be two lung problems to deal with.
- The size of the lungs. Lungs that are smaller than normal are hypoplastic. This means the lungs are underdeveloped. The lungs may not be large enough to sustain life. This condition is called pulmonary hypoplasia.
- Abnormal blood pressure in the lungs. This is called pulmonary hypertension. We watch to see how well your baby can take in oxygen and remove carbon dioxide through their lungs.
Pulmonary hypertension
Pulmonary hypertension is a life threatening complication. If the oxygen levels are low, your baby may need more aggressive treatment. This may include nitric oxide therapy and a heart bypass machine.
- Nitric oxide therapy
During nitric oxide therapy, the oxygen supplied to the baby is enhanced with a gas called nitric oxide. This gas goes right into the breathing tube used to give oxygen to your baby. - Heart lung bypass (ECMO)
ECMO is a type of heart lung bypass. While on ECMO, the heart and lungs are able to rest because the machine does their work. This rest sometimes gives time for pulmonary hypertension to get better on its own. ECMO is used when other treatment options do not work.
When will surgery be done?
Doctors will close the diaphragm if and when your baby is well enough to have surgery. You may need to make some very hard decisions during this time.
What happens after surgery?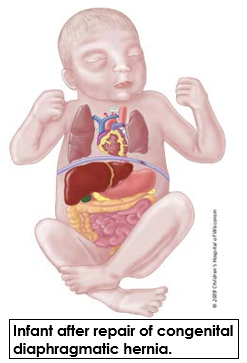
After surgery your baby will still need help to breathe well. Lab work to check oxygen levels, electrolytes and blood counts will be done often. After surgery your baby may need many medicines, including:
- Antibiotics to fight infection.
- Medicine to control pain.
- Medicine to even out and keep a high enough blood pressure.
- Sedation to keep your baby calm.
- Paralytics to keep your baby from moving.
Your baby may look puffy or swollen after surgery. Your baby will not be able to eat until they are stable. Your baby will get IV fluids and nutrition.
Because infants with CDH cannot eat for a long time, special nourishment will be given through a central line. Total parenteral nutrition (TPN) is an IV solution that has protein, fats, sugar, vitamins, and minerals. TPN gives all the nutrition needed until your baby is able to take food by mouth.
Before starting feedings by mouth, there will be signs that your baby’s bowels have started to work. Signs include bowel sounds, pooping, and less drainage coming from the tube in your baby’s stomach. Feedings may go through the tube that is in your baby’s stomach. Your baby will start with a very small amount. The amount is slowly increased as your baby tolerates the food. In babies who need to be fed through a tube, our goal is to move to feedings by mouth if your infant is able.
Will I be able to help care for my baby?
Yes. Please ask your baby’s nurse how you can interact with and care for your baby. If you had planned to breastfeed your baby, you can start to pump while you are still in the hospital. Breast milk is often the best nutrition for your baby. A lactation consultant can answer your questions. Your milk will be frozen and stored in the NICU until your baby is ready for it. The NICU has breast pumps and private rooms you can use when you are visiting.
When can my baby go home?
Your baby will go home when they can eat enough to gain weight and your baby’s lungs are able to take oxygen to the body. Every baby is different. The average length of stay is 6 to 12 weeks.
What is my baby’s long-term prognosis?
Long-term issues include chronic lung disease and gastroesophageal reflux. Babies with CDH will be checked for developmental delays. The long stay in the hospital and breathing difficulties can cause these delays.
For those who do not need ECMO, the survival rate is about 90 percent. If your baby requires ECMO, the survival rate is about 50 percent.



