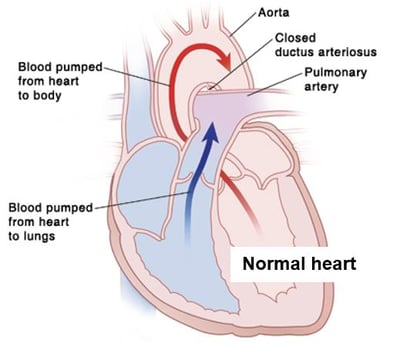
The ductus arteriousus is a blood vessel that connects two arteries, the pulmonary artery and the aorta. The pulmonary artery carries blood from the heart to the lungs. The aorta carries blood from the heart to the body.
The ductus arteriosus normally closes shortly after birth. It’s called a PDA when it stays open, or patent.
The PDA is a normal structure in the fetus. While in the womb, the baby does not breathe. That means only a little blood needs to go to the baby’s lungs. The PDA allows blood to flow from the pulmonary artery to the aorta, bypassing the lungs.
Why is a PDA a problem?
- With a PDA, blood flows from the aorta through the PDA into the pulmonary artery. This causes increased blood flow to the lungs. If the PDA is large, too much blood goes to the lungs and the baby has a hard time breathing and feeding.
- In severe cases, both the increased blood flow to the lungs and the extra work the heart needs to do can lead to congestive heart failure (CHF). This is a condition in which the heart no longer pumps blood well.
What are the symptoms?
Most children with a small PDA have no symptoms. Children and infants with large PDAs are more likely to have symptoms. These can include:
- Trouble breathing.
- Trouble feeding.
- More sweating or tiredness than normal.
- Slow weight gain.
- Frequent lung infections.
- A heart murmur.
- Low blood pressure or a wide range of blood pressures.
- Increase in the baby’s heart rate.
How is it diagnosed?
Heart problems in children are usually diagnosed and treated by a doctor called a pediatric cardiologist. Signs of a heart problem will be checked for during a physical exam. To confirm a diagnosis or learn more about a possible heart problem, several tests may also be done. These include:
- Chest X-ray: Shows the lungs and heart.
- Electrocardiogram (EKG): Records the heart’s electrical activity.
- Echocardiogram (echo): Creates a moving picture of the heart.
How is it treated?
A PDA may close on its own without treatment. If it does not, treatment options depend on your child’s age and the size of the PDA. Options include:
- Medicine. (Newborns only) Some medicines can narrow the artery, shrinking the duct and allowing it to close. Medicine is given by IV over a period of a few days. During this time, the baby is watched closely.
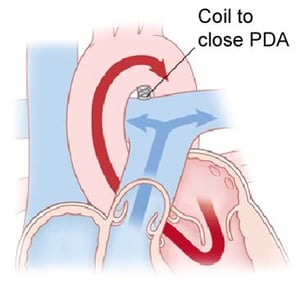
- Cardiac catheterization. A thin, flexible tube (catheter) is inserted into a blood vessel. It’s used to guide a coil into the heart to close the PDA. The catheter is removed once the coil is in place.
- Surgery. An incision is made in the left side of the chest, between the ribs. The ductus is closed by tying it with a suture (thread-like material) or by permanently placing a small metal clip around the ductus to squeeze it closed.
Your child’s cardiologist will evaluate your child’s heart and discuss the best treatment option with you.
Risks and possible complications of cardiac catheterization or surgery
- Reaction to contrast dye. This is only with cardiac catheterization.
- Reaction to sedative or anesthesia.
- The PDA does not close completely.
- Infection.
- Bleeding.
- An abnormal heart rhythm called arrhythmia.
- Injury to the heart or a blood vessel.
What are the long-term concerns?
- After repair of a PDA, symptoms related to the defect should go away. Your child’s heart should work normally.
- Follow-up visits with the doctor may be needed.
- To prevent infective endocarditis, your child may need to take antibiotics before having any surgery or dental work. Antibiotics should be taken as directed by the cardiologist.