Understanding Tracheostomies
- What is a tracheostomy?
- What is a tracheostomy tube?
- Why does my child need a trach tube?
- What extra care must I take to keep my child safe?
- What happens after surgery?
- When will my child be ready to go home?
- What follow up medical care will my child need?
- Will my child be able to talk?
- Will my child need to be monitored at home?
- Will my child be able to do the same things a child without a trach can do?
What is a tracheostomy?
- A tracheostomy, or trach for short, is an opening in the windpipe (trachea). Your child will breathe through the trach instead of through the nose or mouth.
- The doctor made a small opening in your child’s neck during surgery. It is called a stoma.
- The trach stoma lets air and oxygen pass through the windpipe into the lungs.
- Extra secretions are removed from the windpipe through the trach tube.
What is a tracheostomy tube?
- A tracheostomy tube is a short, soft, flexible plastic tube that goes into the windpipe through the stoma. It is smaller than the inside of the windpipe, so your child will not feel it.
- The trach tube keeps the windpipe open so your child can breathe easily.
- The amount of sound made is affected by the amount of air your child can breathe around the trach tube. This is because the air travels out of the stoma instead of through the vocal cords (where sound is made) and out the mouth.
Why does my child need a trach tube?
- Your doctor will talk with you about why your child needs a trach tube.
- Your child may need a trach to keep the airway open and help their breathing due to:
- Birth defects that affect breathing.
- A windpipe or breathing tube that is narrow or scarred.
- Vocal cords that don’t move like they should.
- A problem such as softening or collapse of the windpipe or bronchial tubes.
- A need for a ventilator to help with breathing.
- A disease that affects the muscles or nerves that control breathing.
- Often the trach is not permanent. It may be able to be removed when your child grows or when the problem is corrected.
What extra care must I take to keep my child safe?
- Your child with a trach needs to be watched closely day and night.
- A trained adult caregiver must be with your child at all times. This person must be trained in suctioning, trach cares, trach tie changes, and changing the trach tube.
- The trained adult caregiver must also be trained in trach CPR.
- All caregivers need to practice good hand washing before and after caring for your child. This will reduce your child’s risk of infection.
What happens after surgery?
When will my child be ready to go home?
Your child will be ready to go home when:
- They are medically stable.
- You and other caregiver(s) are fully trained in providing care.
- Home support agencies are in place.
What follow up medical care will my child need?
After discharge, your child will need follow up medical care from the:
- Pediatrician for routine child care.
- ENT doctor who performed the tracheostomy.
- Pulmonary doctor in the Tracheostomy Clinic.
The nurse on the Tracheostomy Team will coordinate your child’s follow up care.
Will my child be able to talk?
The trach tube will not keep your child from learning how to speak. There are some things that will affect the amount of sound your child will make:
- The size of the trach tube.
- The amount of air your child can breathe around the trach tube.
- Air is exhaled through the trach tube instead of the vocal cords, mouth, and nose. This means your child’s voice will be soft.
- Many children are able to use a “speaking valve” to help learn to communicate. Speech therapy and the trach team will work to assess your child for readiness to use this valve.
In the hospital and after discharge, your child will have speech therapy to help with talking.
Will my child need to be monitored at home?
Will the trach change the way my child eats?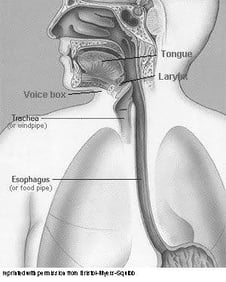
The trach tube does not affect the way your child eats food.
Some children who have trach tubes have a hard time with swallowing and gastric reflux. Because of this, some children are at risk to aspirate (inhale) food into the airway.
If your child has feeding or swallowing issues, your doctor will talk with you and decide if tube feedings will help prevent reflux or food aspiration.
Will my child be able to do the same things a child without a trach can do?
Will my child be able to leave the house?
Yes, your child will be able to leave the house and travel with the family. All the equipment you need is portable or will work on battery power. You will learn which pieces of equipment you need to have with you at all times when you and your child go out of the house.
What training is needed? 
Family and trained caregivers
As you are getting ready to take your child home, you will need the help of the trach team members. More importantly, you will need the support and help of family and others.
An adult caregiver who is trained to do routine and emergency trach care must be with your child at all times.
Many of the cares need two people to perform. You will need at least one other adult to be completely trained in your child’s care. This second caregiver will learn as much about your child’s care as you have. This person should be an adult who will continue to be involved in your child’s life after discharge. This person will spend time with your child and be a resource and back up person for you when you cannot be with your child.
Daily cares and home equipment training
Before your child can go home, you and the second caregiver will need to learn and demonstrate the care that your child needs.
Training includes learning about your child’s:
- Physical care
- Care of the tracheostomy
- Giving medicines
- Feedings
- Equipment care
You will work closely with the nurses and respiratory therapists to learn how to:
- Suction
- Do trach care
- Change trach ties
- Change the trach tube
- Give breaths with the resuscitator bag
Simulation training and independent cares
Before going home, you will use all the skills you have learned to complete simulation training. You will work together to act out emergent scenarios on a doll, using home equipment.
Then you will do independent cares before your child goes home. This means that while you are still in the hospital, you and the other trained caregiver(s) will provide all the care your child will need at home. You will need to do this in separate shifts from each other.
You will spend 6 to 24 hours doing all the cares for your child. You will use your child’s own home equipment and supplies.



