In this section
Questions to ask your child's heart center
It's hard to hear the words, "There is something wrong with your baby's heart." But there is hope. Thanks to new and better treatment, your baby's chance of surviving is better with the right care.
After receiving a diagnosis, many families don't know the questions to ask when selecting a cardiac care center for their child. To help guide families through this difficult time, the Conquering CHD (formerly Pediatric Congenital Heart Association), a parent-led national organization and advocacy group, developed the Guided Questions Tool to help families make more informed care decisions and select the best cardiac care center for their child.
In an effort to be as proactive and as transparent as possible for families, the Herma Heart Institute (HHI) has supplied answers for each of the Conquering CHD's questions and are available below. Throughout this page, additional videos are available featuring HHI and Conquering CHD staff that will provide more detail to the questions and answers provided.
Because this information may be unfamiliar or hard to understand, we strongly encourage you to ask questions of your cardiologist or care team so they can help clarify.
Download a copy of the Herma Heart Institute's answers to the Guided Questions Tool.
Watch: What is the Guided Questions Tool?
What is the Guided Questions Tool and why and how was it created? Hear from Amy Basken, Director of Programs at the PCHA, and Julie Lavoie, Quality Improvement Manager at the Herma Heart Institute, talk through the history of the tool and their vision for every pediatric heart program to proactively provide answers to the questions.
Table of Contents
![]() Questions to ask about your cardiac center
Questions to ask about your cardiac center
Questions to ask about your cardiac center
Questions 1 and 2:
- How many procedures do you perform each year?
- How many times have you and your program performed this procedure or ones like it in the last year? Over the last 4 years?
- What is the survival rate for this type of procedure at the time of hospital discharge? After one year?
- How do your results compare to other centers' results?
A closer look at cardiac surgical data
Questions like "How many procedures does your center perform every year?" seem like they'd be easy to answer. Hear from Julie Lavoie on the many ways a program can provide data to answer the question and how the Herma Heart Institute chose to answer.
On average, Children's Wisconsin performs over 550 pediatric and congenital heart surgeries each year. Children's is considered a high-volume center by the Society of Thoracic Surgeons (STS). STS created a national database to track patient quality and safety measures and reports volumes and outcomes from over 110 pediatric heart centers across the country. Children's has been reporting volume and outcomes to the STS database since 2004 and consistently ranks among the top programs in the country.
Below are our surgical volumes from 2016-2019:
Cardiac catheterizations may be used to assess and/or treat some heart conditions. We perform about 500 procedures in the cardiac catheterization lab each year. This includes both cardiac catheterizations and electrophysiology (EP) procedures. During cardiac catheterizations, x-ray equipment, special dye (contrast) and long, flexible tubes (catheters) are used to visualize blood flow through the heart and vessels. These catheters are special in that they allow interventions upon structures within the heart, such as valves or blood vessels. Catheter procedures are less invasive than open heart procedures. Your doctor will let you know whether catheterization is needed for your child's condition. Electrophysiology procedures done in the catheterization lab also use specialized catheters. These catheters help to diagnose, map, and treat the origin of abnormal rhythms.
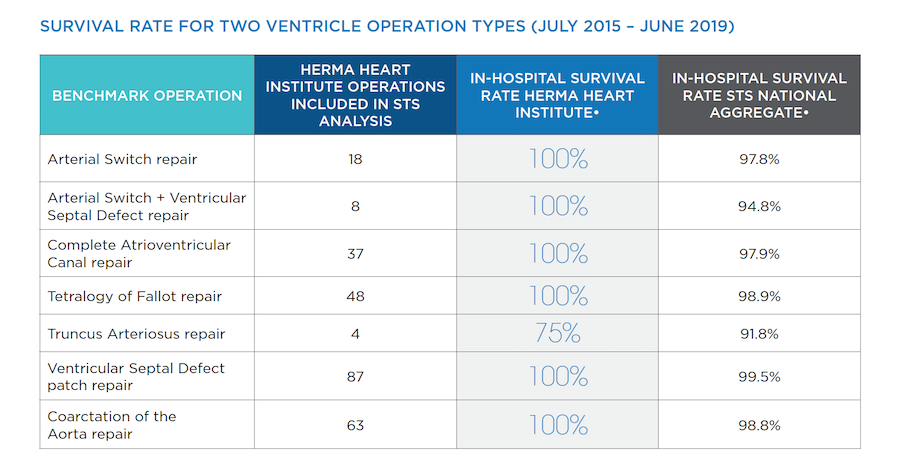
Below is a list of operations that STS refers to as benchmark operations. Please note that operations for patients with single ventricle anatomy are part of the benchmark operations but are displayed in their own table. The national survival rate for these operations is shown, based on data from the Society of Thoracic Surgeons (STS).
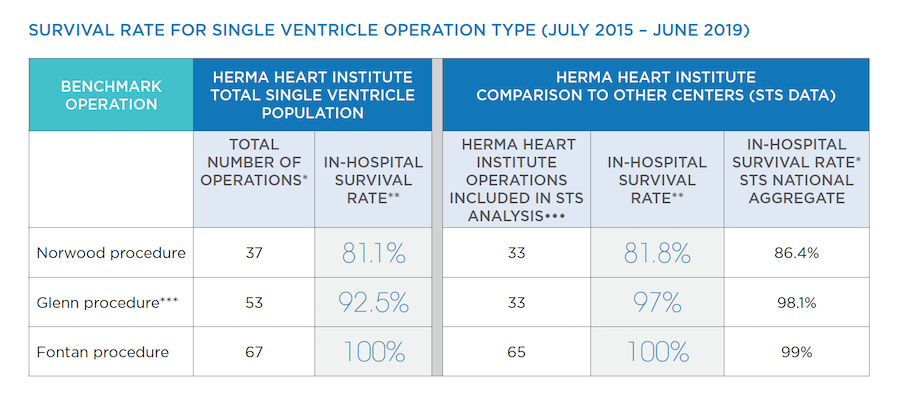
*In-hospital survival rate means that infants survived at least 30 days after surgery and through discharge from the hospital.
*Total number of operations – The left hand side of this chart shows the total number of operations performed at the HHI. When analyzing and comparing outcomes between centers, the STS only counts an operation when it is the first one during a child’s hospital stay. Often the sickest babies need to have a temporary procedure to allow them to get better before undergoing the Norwood procedure and so their Norwood isn’t counted in the STS report. Also, many patients who do not go home between Norwood and Glenn are the most medically fragile. They are not counted in the STS report. In order for you to understand how our outcomes compare to other centers, the right hand side of this chart includes the patients that STS includes in their analysis with survival rates both at our center and all combined STS centers.
**In-hospital survival rate means that infants survived at least 30 days after surgery and through discharge from the hospital.
***Patients who had Glenn and Norwood procedures during the same hospital admission are only categorized as Norwood in the STS data.
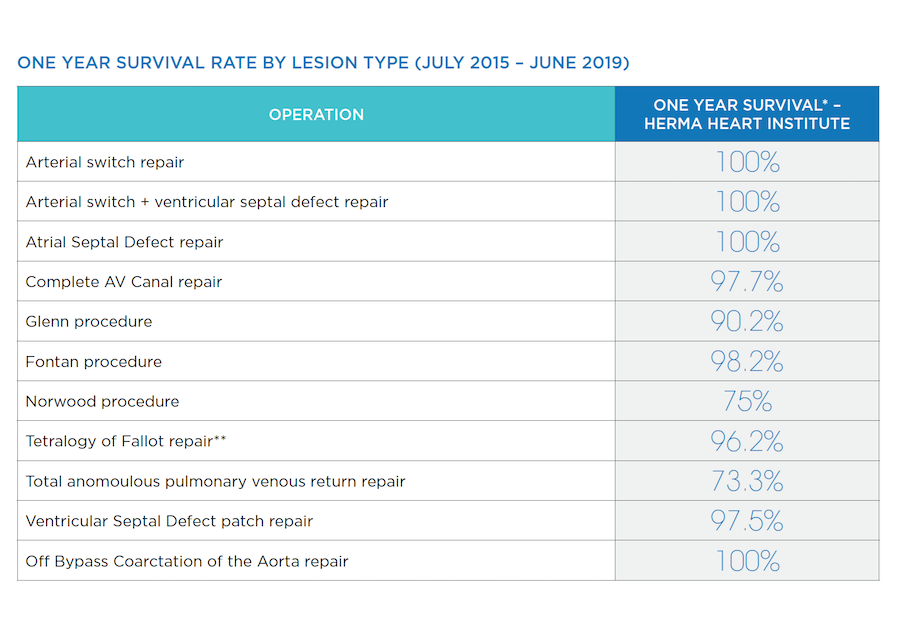
*One year survival rate includes only patients from Wisconsin because we are not able to track patients who come from other states. STS does not currently report one year survival rates across centers.
**Tetralogy of Fallot – this category does not include those patients with pulmonary valve atresia, absent pulmonary valve, atrioventricular canal, and major aortopulmonary collateral arteries.
Question 3: What are the most likely complications or three things that can go wrong with this procedure and how often do they happen within one year of this procedure?
Bleeding, abnormal clotting, feeding difficulties, abnormal heart rhythms and infections are the most common complications that are seen in our cardiac population after surgery.
- Bleeding typically slows down and then stops within the first few hours after surgery. If that doesn't happen, our team will give your child medicine that will help stop the bleeding. In rare cases bleeding will not stop, or will become worse. If this happens, your child may need to be given a blood transfusion and may need another operation to stop the bleeding.
- Abnormal clotting is another post-operative risk. For our patients that form abnormal clots, medicine can be given to break apart the clots and prevent them from causing an obstruction. Sometimes patients need to stay on medicine for several weeks to assure their risk of abnormal clot formation is resolved.
- Feeding difficulties occur with some babies who undergo heart surgery. This may be a result of injury to the nerves that control the vocal cords that occurs during the operation or due to the development of poor oral motor coordination during hospitalization. We have a specialized team of dietitians and speech therapists that work with patients to provide nutrition support and feeding skill development. Some babies require tubes to be placed through the nose into the stomach for feeding. Occasionally babies may need a tube placed surgically into the stomach for nutrition to be given at home.
- Abnormal heart rhythms, or arrhythmias, can happen after heart surgery if the heart is irritated by the procedure. Most arrhythmias get better in a few hours or days after surgery and do not cause problems later. When an abnormal rhythm persists, our team prescribes medicine to control the abnormal rhythm. Rarely, a pacemaker may be required. This device helps your child's heart have a regular rhythm. If your child has arrhythmias or needs a pacemaker, they will be seen by the Herma Heart Institute's Electrophysiology Program. The program is the largest in the state and has electrophysiologists who are specialists in arrhythmias.
- Infections following surgery are rare. The hospital tracks all surgical site infections very closely and treats them aggressively. All of our patients receive antibiotics before and after surgery to help minimize the possible risk of infection.
Question 4: Do you share your results with national data programs such as the STS Database or IMPACT Registry to help improve care? Is this information open to the public?
We were one of the first pediatric heart centers to endorse the public reporting of data to share information with families. We believe that sharing outcomes empowers families in decision making and helps centers improve care. This helps to make sure we are working towards the best care for our patients and their families.
We share our data with more than a dozen national data registries, including:
- The Society of Thoracic Surgeons (STS) database for surgical outcomes. This includes 119 Congenital Heart Disease programs in North America that report on outcomes by procedure type and complexity. Our outcomes are shared publicly on the STS public outcomes page. Comparison of outcomes between centers allows us to compare ourselves with other centers and ensure that we are providing the best and safest care.
- The IMproving Pediatric and Adult Congenital Treatments (IMPACT) database for cardiac catheterization outcomes. This registry allows us to compare our data with other pediatric cardiac catheterization programs to ensure we are providing excellent care to our patients.
- The National Pediatric Cardiology Quality Improvement Consortium (NPC-QIC) for patients undergoing the Norwood procedure for Hypoplastic Left Heart Syndrome. Groundbreaking improvement in care for patients with Hypoplastic Left Heart Syndrome at Children's Wisconsin dramatically improved survival in patients between surgical procedures (see Interstage Monitoring in question 7 below). Recognition of the importance of these changes led to formation of the NPC-QIC. Children's continues to participate in NPC-QIC and is a leader in pushing for transparency of outcomes within this consortium.
Question 5: Do your surgeons have special training in congenital heart surgery? What other types of special training do your doctors and nurses have?
Our three cardiothoracic surgeons are board certified and sub-specialty trained to perform pediatric congenital heart surgery.
Each of our surgeons has decades of experience in pediatric cardiothoracic surgery, and each is nationally recognized.
The Herma Heart Institute is home to a multi-disciplinary team of experts. Our experts cover the full spectrum of cardiac care: fetal cardiology, cardiac intensive care, cardiac anesthesiology, cardiac catheterization, cardiac imaging, electrophysiology, cardiogenetics, pediatric psychology, clinical nutrition, perfusion, developmental follow-up, school intervention, adult congenital heart disease, and more. Talk with our providers to learn how these experts can be involved in your child's care.
Question 6: How are family members included in the decision-making process? How will the care team give me information or reports before, during and after the procedure?
Parents are the most important people in a child's life. We want to include you in every part of your child's care. This partnership starts as soon as your child's diagnosis has been determined, which is often prenatally. You will have a chance to learn about how we are doing (our outcomes), take a tour of our hospital, and meet with members of our team.
If your child needs heart surgery, you will have a meeting with the surgeon. He will be able to answer any of your questions before the surgery. On the day of surgery, our cardiovascular nurse clinicians will keep families updated every hour on how the surgery is progressing. For any child who will be staying with us after surgery, families are invited to bedside rounds. At rounds, you are invited to ask questions and are encouraged to be involved in planning your child's care. Upon discharge, you will be provided with education for care at home as well as a plan for future clinic appointments and referrals to any sub-specialty that may be necessary for your child to achieve their highest quality of life.
Questions to ask about your hospital stay
Question 7: How many days do you think my child will be in the hospital, both before and after the procedure?
* ASO – arterial switch operation; VSD – ventricular septal defect; CAVC – complete atrioventricular canal; TOF – tetralogy of fallot; TA – truncus arteriosus; CPB – cardiopulmonary bypass; CoA – coarctation of the aorta; Median lengh of stay means that half of our patients go home before that number of days in the hospital and half of our patients go home after that number of days.
Median length of stay means that half of our patients go home before that number of days in the hospital and half of our patients go home after that number of days.
Interstage Home Monitoring Program
One example of our commitment to success is our Interstage Home Monitoring Program. For babies with shunt-dependent pulmonary blood flow, there is a critical period in between the Norwood and Glenn procedures called the interstage period. Your baby needs extra monitoring at home to prevent serious problems. The Herma Heart Institute developed the Interstage Home Monitoring Program to help support parents in the at-home setting. In just one year, this program reduced mortality rates from 15% to 0%. We are proud to say that we have maintained these survival rates throughout the last ten years. Today, this program is a national standard of care.
Question 8: What are my options for when, where and how to deliver my baby? How do you work together with my OB/GYN/midwife to prepare for my delivery and my care right before and after delivery?
When: Your baby's heart disease does not typically affect the timing of the birth. The goal is for you to give birth to a full term infant. If you do not live in the Milwaukee area, we may have you plan to come in and induce at 39 weeks pregnancy. Again, your provider will help plan for this if needed.
Where: The location of delivery depends on when we expect your child to need a procedure. If your baby is not expected to need surgery in the first weeks after birth and you do not live in the Milwaukee area, most babies can deliver closer to home with care from their primary doctors. Our fetal cardiology team will discuss this with the referring physicians, to make sure they are comfortable with this plan, and to organize follow-up after birth.
For babies who may need a procedure in the first weeks after delivery, we recommend you give birth at Froedtert Hospital's Birth Center. The birth center is located within Children's Wisconsin, and is adjacent to the Level IV neonatal intensive care unit (NICU) A Level IV NICU is the highest rating given by the American Academy of Pediatrics, and is given to pediatric hospitals that care for the most complex babies. We are one of the few major heart centers that has an in-house delivery unit, avoiding difficulties associated with transport of critically ill newborns. If you plan to deliver at Froedtert's Birth Center, we will ask that you be seen by the high-risk obstetrics (OB) team at Froedtert Hospital so that they can plan your delivery. Our fetal cardiology team meets with Froedtert's high-risk OB team to ensure the care is coordinated for both mom and baby.
How: We anticipate a vaginal delivery in most cases. However, if the fetal cardiologist feels that your baby will need immediate intervention for stabilization, we may recommend a C-section. Your provider will talk with you if that is the case.
Question 9: How do you work together with my baby's doctor after birth and after the procedure?
We know a family's relationship with their baby's pediatrician is special. We partner with your baby's doctor and send them updates to keep them informed about your baby's condition and the care required.
After you go home from the hospital following delivery, your baby's cardiologist will work closely with your pediatrician to coordinate care. If you have concerns about your baby's health, call our office to speak with a nurse or the on-call doctor. We can talk about your concerns and how to help.
Question 10: If my baby needs to stay in the hospital after delivery to prepare for a procedure, where will he/she be? What about after the procedure? Do you have a cardiac intensive care unit (CICU) that cares mainly for children with heart defects?
Before and after surgery
Babies who need surgery before going home will usually be admitted to our Level IV NICU (see answer #8 for why a Level IV NICU is important). Before the scheduled surgery, your baby will move to our cardiac intensive care unit (CICU) for pre-operative care. This allows our CICU team get to know you and your baby. After surgery, your baby will return to the CICU. As he/she heals and gets closer to going home, he/she may be moved to a special unit that cares for recovering cardiac babies.
Our Cardiac Intensive Care Unit
Our CICU is staffed around the clock by highly experienced, board-certified intensive care specialists with additional education in cardiology, cardiac intensive care and cardiac anesthesia. Our team is on the cutting-edge of improving critical care outcomes, specifically in the areas of post-operative care in protecting brain and kidney function. We have also pioneered methods for monitoring how well the heart is delivering blood to the body.
Question 11: Will I get to hold my baby before or after the procedure? If so, when and how?
Our priority is your baby's safety. Often parents can hold their baby prior to the procedure, and within a few days after the procedure. Our skilled nursing staff will promote as much interaction with your baby as possible and ensure that you are closely involved with their care.
Question 12: Will I be able to breastfeed my baby after delivery and again after the operation? Will my baby require a special diet? Should I expect my baby to take a bottle or breast feeding without problems?
We promote breastfeeding your baby both before and after the procedure whenever it is safe. We have developed a set of guidelines to determine if this is right for your baby. We also involve our feeding team from the start, to give your baby the best chance at feeding normally. The team includes specialists, registered dietitians and speech-language pathologists, who will create a personalized plan based on your baby's specific needs.
Our team of certified lactation counselors can support you and your baby in breastfeeding. Children's also has a state-of-the-art milk kitchen which can add extra nutrients to your breast milk, if needed, to help your baby grow.
Question 13: What do you do to help prepare parents to take their babies home from the hospital?
Our goal is to educate families well in advance of hospital discharge, so that there is a safe and smooth transition to home. Each baby is provided with a care plan unique to their medical and developmental needs. Our care providers work with families, educating them on the many aspects of cardiac care so that parents feel empowered and comfortable caring for their baby in the home setting.
Teaching parents
From the moment your family becomes part of the Herma Heart Institute, our cardiac team will find ways to involve you in every aspect of your child's care. We prioritize parental involvement because we believe it helps families become more confident and it builds a positive environment for everyone involved.
Our nursing staff partners with you, teaching you necessary skills required to care for your baby at home. They will give your family hands-on guidance and practice so you are well-prepared to take care of your baby's daily needs like feeding and giving medicine.
While your baby is here, you will learn about their care, nutrition, safe sleep, CPR and how to use a car seat. You may also be approached to participate in research studies or quality of care projects. We ask for participation from our families so we may continuously strive to provide excellent care. Our Family Resource Center, on the first floor of the hospital, can also help parents find resources and parenting programs.
Before you go home, you may also have time to “room in.” For patients enrolled in our interstage program, this is a mandatory part of the discharge process. During this time, you will manage all of your baby's care for 12-24 hours. This will help you become more comfortable with your baby's needs while the care team is nearby to answer questions and assist.
When you go home, you will leave with teaching sheets, a medicine list and a visit summary which clearly explains how to reach the heart team if you have any questions or concerns.
Managing needs
Often, our patients need the support of more than one specialty, and the Herma Heart Institute team will help you coordinate the care for your baby after they go home. Here are some ways we work with other specialties to get your baby ready for home:
- Physical and occupational therapy (PT and OT): Through routine therapy sessions, our physical and occupational therapists will work with you to create goals for your baby's mobility and range of motion. We offer these services both in the hospital and in an outpatient clinic as needed.
- Feeding and nutrition: A feeding and nutrition team member is present during bedside rounding while your baby is in the hospital. The CICU has specific care providers that are experienced in working with heart babies and their specific nutritional and feeding needs.
Our feeding team includes a pediatric speech-pathologist and registered dietitian. They work together to create a personalized feeding plan for your baby. This plan includes special recipes, feeding schedules, and oral-motor exercises designed to achieve proper growth. Parents' needs and concerns are considered when making the plan. This helps prepare you to follow the plan at home. As your baby makes progress, the feeding and nutrition team will keep working closely with you to adjust and advance the feeding plan. If your baby does require nutrition support in the form of a feeding tube, our team will continue to work on feeding skills and support a move to oral feeding at the right time.
- Complex Care Program: The Complex Care Program helps coordinate medical and non-medical services for children with complex needs. The care team works with family, doctors, community resources, and insurers to make sure your baby is getting the best care in and out of the hospital through individualized care plans. They work to coordinate multiple appointments on the same day and streamline medically complex plans into a simple care plan that works well at home.
Supporting after discharge
During your stay, we will work to coordinate care with your baby's primary care provider. Any follow-up appointments will be scheduled and shared with you before discharge. You will receive a printed list of these appointments.
Case managers can suggest resources to help with your family's specific physical, emotional and financial needs. They work with Herma Heart Institute social workers and your baby's heart team to coordinate any services you may need after discharge. This may include home nursing, medical supplies, home therapies, or specialty services.
Question 14: What support is available for me and my family? For example, can I talk to other families that also have children with heart defects? Do you provide financial, nutritional, and mental health support?
This is an incredibly stressful time in a family's life, and we want to be as supportive and share as many resources as we can to help you through the unknown. Many parents find it helpful to connect with other parents who have children with heart conditions, and so we often connect families with each other. This often occurs at the first prenatal visit. There are also many local and national parent groups that focus on families affected by congenital heart defects, including the Pediatric Congenital Heart Association and Mended Little Hearts. These groups offer peer-to-peer support services. They also share information and promote awareness and advocacy. Our providers and care staff are active volunteers and contributors to these communities.
A team of support
We offer resources and a variety of teams built to support your family during this stressful time:
- Social workers: Our team of social workers is ready to connect you with the programs and services you need. We help you partner with other heart families through local programs such as Mended Little Hearts and Parent 2 Parent of WI. We can also connect you to Financial Counseling services, where financial counselors guide families and patients on how they may secure insurance and explore various options for covering the costs of services at any of our Children's locations.
- Registered dietitians: As part of the feeding team, our dietitians care for your baby in both the inpatient and outpatient setting. They manage your baby's feeding plan to make sure your baby is meeting nutrition and growth goals and provide nutrition support when your baby is unable to meet their calorie goals orally.
- Psychologists: Our psychologists support your baby and family's well-being. They can do assessments and provide therapies for children with developmental and behavioral concerns. (Our psychologists support our Developmental Follow-Up Program, which you can learn more about in answer #16.)
- Child life specialists: Our child life specialists support both patients and their siblings with helpful ways to cope. They do this through play, preparing for procedures, teaching aimed at the child's level of learning, and using self-expression activities.
- Chaplains: Our chaplains offer spiritual, religious, and emotional support to children and families of all faith traditions.
Questions as you're looking ahead
Question 15: What are the expected long-term results for this heart defect and its procedure? What is my child's life expectancy or how long is my child expected to live? Are there other possible lifelong problems that I need to watch out for?
Long-term outcomes vary based on your child's specific condition. Some heart defects can be fixed with one operation, while for other defects additional surgeries may be needed as children get older. This will depend on your child's diagnosis.
Understanding your child's heart defect
To have the best understanding of long-term outcomes, it is important to talk with your cardiologist. It is also important to understand the limits of a prenatal diagnosis. Unfortunately, we do not always have all of the answers about your child's diagnosis before birth. While we can find many issues in utero, the way the blood flows through the heart changes after your child is born and starts to breathe. For certain heart conditions, it can be difficult to predict how the heart will handle those changes. More testing may be needed after birth to understand all the details of your child's condition.
Focusing on quality of life
For children with complex heart defects, movement, play, feeding and language skills may develop more slowly. Some children with heart defects may need extra help in school or have emotional or behavioral challenges.
Because the outcomes of surgery for heart disease have greatly improved over the past twenty years, the goal of the Herma Heart Institute has moved beyond survival after surgery. We now focus a great deal of effort on making sure that heart kids experience a high quality of life. Some of these efforts have grown into full programs, like our Developmental Follow-Up Program, School Intervention Program and Steppin' It Up Program. Learn more about these programs in answer #16.
Improving outcomes through adulthood
More and more, children with congenital heart defects are living longer into adulthood. New complications can occur as a result of the original heart defect. The Herma Heart Institute created the Adult Congenital Heart Disease (ACHD) Program to respond to these new challenges. Learn more about the ACHD program in answer #17.
Question 16: Thinking about how my child will grow and develop, what should I expect from them as a preschooler, school-age child, a teenager and as an adult?
Our team is devoted to helping your baby grow into a healthy adult and have lifelong success. Here are a few programs we offer to children and their families to improve quality of life:
- Developmental Follow-Up Program: For many reasons, skills such as talking, crawling, and playing may develop more slowly in children who have had heart surgery or intervention for complex congenital (present at birth) heart defects early in life. Our developmental experts include specialized developmental pediatricians, psychologists, nurses, and occupational, physical, and speech therapists. They work closely with your child, especially during the important first three years of life, helping you watch for developmental delays and advancing your child's skills in many areas. We suggest that all children who have had a heart surgery as babies participate in the program, even if they appear to be healthy and doing well.
- Steppin' It Up Program: Children with heart disease and their families sometimes have a great deal of anxiety about taking part in physical activities. This can impact their long-term health and quality of life. Our Steppin' It Up Program helps patients develop the skills they need to safely do physical activities and improve self-confidence. In this yearlong program, patients advance through three tiers, and have the support of experts in cardiology, exercise physiology, psychology and physical and occupational therapy.
- School Intervention Program: Children with congenital heart defects are at risk for delays in learning. To make sure our patients and families have the support and resources they need to reach their full potential, we developed our School Intervention Program. Since 2015, children from kindergarten through college have used this program. We assess each patient's educational needs and goals, and create personal academic plans by working with their school. Our school intervention specialist serves as a consistent link between the hospital, family and school, providing clear communication.
Question 17: As my child gets older, does your medical care provide a plan for transitioning from pediatric to adult care?
We have a formal transition process in place to prepare adolescents for transition to our Adult Congenital Heart Disease (ACHD) Program as they move from childhood to adulthood. The move from child-centered to adult-centered care is a gradual process that The Herma Heart Institute calls the Transition Program. Successful transition begins during the adolescent years, and ensures patients continue to receive specialized cardiology care and lifelong monitoring.
Members of the Transition Program work with each patient's pediatric cardiologist to ensure uninterrupted health care that is patient-centered, age and developmentally appropriate, flexible, and comprehensive. Transition visits start around age 16 and continue yearly until transfer of care to the ACHD program. Fortunately, patients cared for at Children's can continue their cardiology care within the same hospital they have visited for years.
Our ACHD program is the largest in the state and one of the largest in the nation. All of the team's cardiologists are board certified in adult congenital heart disease. Today, more than 2,600 adult congenital heart patients are followed in the program. Our ACHD program meets the highest standards of ACHD care and therefore is nationally accredited as an Adult Congenital Heart Association Comprehensive Care Center.
Herma Heart Institute’s answers to the Guided Questions Tool
Download a copy of the Herma Heart Institute's answers to the Pediatric Congenital Heart Association's Guided Questions Tool.
