Help with breathing: After surgery, your baby may not be able to breathe effectively on his or her own due to the increased pressure on the diaphragm from the bowels that are now in the abdominal cavity. We will place a special tube at the time of surgery to assist with breathing (if it was not needed earlier). This tube will stay in until your baby can breathe effectively on his or her own. Typically, babies no longer need support from a ventilator after about 3 days after final closure of the abdomen.
Keeping pressure off the diaphragm: At delivery, we will place another tube into your baby's stomach. This tube will either be placed through the nose, which is a nasal gastric (NG) tube, or mouth, which is an oral gastric (OG) tube. We will apply suction to this tube to keep the stomach empty so as not to cause more pressure on the diaphragm.
Placing IV and other lines: Your baby will not be able to eat for a while after surgery. Some special IV lines will be put in place while your baby is in the operating room for surgery.
- We will place a central IV line so we can give nourishment (vitamins, minerals, calories, fat) for a prolonged period of time.
- We will place an arterial line in one of the arteries in the arm. This is so we can:
- Give IV fluid and medications
- Monitor blood pressure
- Remove blood for lab work
- Before your baby goes to surgery, we will put a peripheral IV in his or her hand.
Drawing blood for testing: Your baby will need frequent blood draws for lab work to monitor oxygenation, electrolytes, blood count and other things. We will place a central IV line so we can give nourishment (vitamins, minerals, calories, fat) for a prolonged period of time.
Medications: Your baby may be on a variety of medications that may include:
- Antibiotics to fight infection
- Pain medication to control pain after surgery
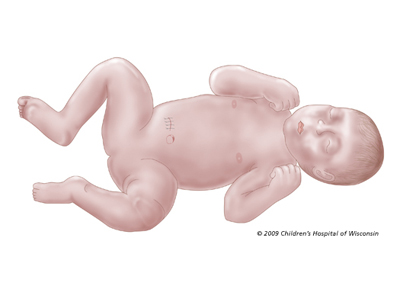
Swelling after surgery: Your baby may look puffy or swollen after surgery. The upper and lower legs may be especially swollen. This is called edema. It will go away as your baby gets stronger and his or her body adjusts to the pressure of the bowels being back in the abdomen.
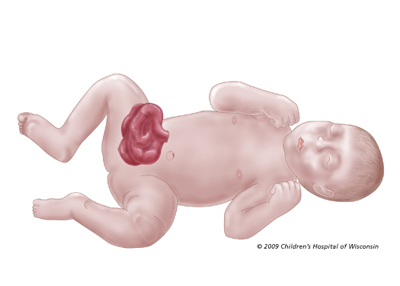
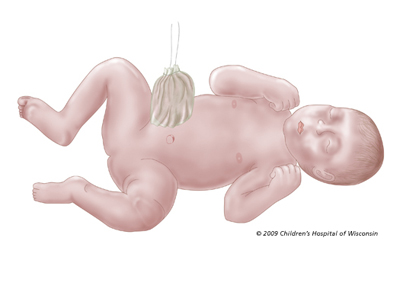
Providing nutrition: Because babies with gastroschisis cannot eat for a prolonged period, special nourishment is given through the central line. Total parenteral nutrition is a solution that contains protein, fats, sugar, vitamins and minerals. This will supply your baby with all nutritional requirements until they are able to take food by mouth.
The hardest part of recovery for babies with gastroschisis is learning to eat and tolerating food. Their bowels were thick, swollen and inflamed at birth, and they require a long time to adjust to having them inside the body. In approximately 10% of infants with gastroschisis, there will be bowel atresias (narrowing). These infants may then need additional surgeries to remove these narrowings to allow normal passage of food.
We wait for signs from the baby that the bowels are beginning to work. These signs include:
- Bowel sounds
- Spontaneous passing of stool
- A decrease in the drainage coming from the tube in the baby's stomach
Feedings usually are started at a slow rate. This rate is gradually increased as your baby tolerates.