Mothers pregnant with monochorionic-diamniotic twins may experience rapid uterine growth, premature contractions and shortness of breath, all signs of excess amniotic fluid. These conditions often start to occur about 20 weeks into pregnancy. If you experience these symptoms, immediately contact your physician.
If the twins' conditions do not require immediate attention, mothers will be closely monitored by ultrasound and fetal echocardiograms throughout pregnancy. Physicians will watch for signs that the cervix is weakening, which increases the risk for premature delivery. They also will monitor the twins for heart failure, soft tissue swelling, abnormal and/or differing fluid volumes and abnormal blood flow in the umbilical arteries. These are all indications that the condition of the fetuses is deteriorating and that additional intervention may be needed.
When excess amniotic fluid is a concern, bed rest or reclining in a horizontal position will be recommended. This will help reduce pressure on the cervix and improve blood flow to the uterus and kidneys. Some research suggests that mothers with pregnancies complicated by TTTS may have lower protein levels in their blood than other pregnant women. It may be recommended that mothers with TTTS pregnancies consider additional protein through nutrition supplements such as protein shakes.
Ongoing monitoring and assessment: The health of the twins is monitored by a perinatologist who will use ultrasound images to assess the progress of the TTTS.
Delivery: This occurs if the pregnancy is beyond 25 weeks and the twins are believed to be healthy enough to survive. If delivery is not an option and treatment is needed prior to delivery, there are three potential approaches.
Amnioreduction: This method is used later in pregnancy or if complications rule out laser ablation treatment. Amnioreduction allows physicians to drain away some of the excess amniotic fluid surrounding the larger twin. This will make the mother more comfortable, reduce the chance of premature labor and better equalize the flow of blood between the fetuses. Amnioreduction is an outpatient procedure and no hospital stay is required unless there are other circumstances that make it necessary. The procedure may need to be repeated through the course of the pregnancy.
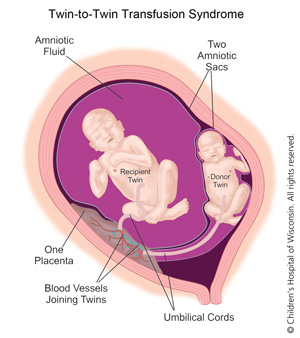
Fetoscopic laser ablation (minimally invasive): Fetoscopic laser ablation of the shared placental vessels is a state-of-the-art and increasingly successful treatment aimed at disconnecting the shared blood vessels between the twins in the placenta. This stops the unhealthy blood transfer between them. Fetoscopic laser ablation is only offered by specially trained physicians at select treatment centers like the Fetal Concerns Center. It is most often conducted between 16 to 26 weeks of pregnancy. Studies show an 80-85% survival rate for at least one twin following laser ablation and an overall twin survival rate of 65-70%. In fact, at Children's Wisconsin, we have a 93% survival rate of at least one baby and 80% survival rate of both babies after laser ablation procedures.* The approach also greatly reduces the risk of neurological damage to the babies before birth.
During laser ablation, a physician inserts a tiny scope (fetoscope) through the uterus to find the blood vessels connecting the twins. The laser seals off the shared vessels so that each fetus now will have their own circulation.
Cord Coagulation: In the most severe cases where there is no chance for the donor twin to survive, a procedure called cord coagulation may be performed. The surgeon will completely close off the blood supply to a failing donor twin so that the recipient twin may thrive. This is considered a last option.
*Based on data from 2012 - 2016.