A bone marrow transplant is a big step — but you won't go through it alone. Our team will be with you and your child every step of the way.
Each BMT is different based on your child and their diagnosis. Your child's care team will walk you through the care plan and what to expect.
Your bone marrow transplant team includes:
- Doctors in oncology, hematology and immunology
- Specialists in infectious diseases, gastroenterology and ear, nose and throat
- Pathologist who examines tissue samples
- An expert in radiation for cancer treatment
- Skilled clinical nurses coordinate care and educate
- Pharmacists to provide medicines
- Dietitians, therapists, pastoral care to support nutrition, physical recovery and spiritual health
- Child life specialist
- Social worker family support
- Transplant coordinator to help you navigate the whole process
Before transplant
The first step for a BMT is to make sure your child is healthy enough. We also work to find the best donor match.
If you find a match and your child is healthy enough, your care team will walk you through the pre-transplant treatment.
Before your child gets a BMT, you'll meet with the Fertility Navigation Program. Kids getting a BMT will need to consider their future family plans. This helps you think through and discuss your child's options for having kids in the future.
Your child will get high-dose chemotherapy and sometimes total body radiation. This destroys damaged or diseased cells, making room for healthy donor cells to grow. This is called conditioning.
Conditioning is an intense process, but it is a critical step to make room for the new bone marrow cells. It takes several days and can cause nausea and vomiting.
It's different for every child, but here's what many families experience:
- Physically tough: Side effects like nausea, vomiting, diarrhea, mouth sores, fatigue and skin changes can be painful or uncomfortable. Your child's care team works closely to keep your child as comfortable as possible.
- Emotionally draining: Your child may feel scared, frustrated or simply exhausted. They may not want to eat, talk or play. You might feel helpless watching them go through it — and that's completely normal.
- Closely monitored: During this time, your child stays in the hospital, often in a special room with infection protection. Nurses, doctors and support staff are always nearby to help.
Bone marrow transplant
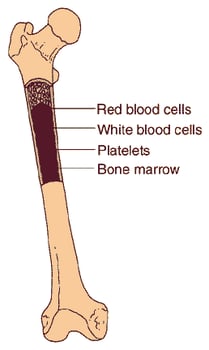
The actual bone marrow transplant is relatively easy compared to the conditioning process. Your child gets the donor stem cells through an IV, just like a blood transfusion. It is not a surgery and usually takes a few hours.
The healthy cells travel to the bone marrow and begin creating healthy blood cells. Transplant day is often called "Day 0" and marks the start of the recovery phase.
After transplant
After the transplant, your child will need close monitoring for infections, bleeding and side effects. They'll take medicines to prevent graft-versus-host disease if the cells come from another donor.
Your child will stay in a special hospital room to protect them from infection while their new cells start to grow. You may be in the hospital for three to six weeks after transplant. Doctors watch for:
- How quickly the new cells start to grow. This is engraftment, which usually happens around two to four weeks after transplant.
- Signs of infection, fevers or other complications.
- How well your child can eat and stay hydrated. They can develop mucositis which are mouth sores or an upset stomach or diarrhea from the chemotherapy or radiation. We will give your child medication to help with any pain and give them nutrition through an IV if that is needed.
You will meet with their care team on a daily basis. Our expert team of nurses will check in throughout the day. They're there to help make sure you have everything you need and feel taken care of.
The MACC Fund Center has resources to make your time with us as comfortable as possible. You can use our:
- Family lounge
- Fully stocked kitchen
- Laundry facilities
Some kids may need a longer stay if they have slow engraftment, serious side effects or graft-versus-host disease. Others may go home earlier if they're recovering well and can be safely cared for nearby with close follow-up.
Survivorship
After you go home, your child will need regular checkups for months or even years. We monitor for side effects and signs of rejection.
Young adults who are currently receiving or have received cancer treatment can get support through our young adult oncology group. The group meets monthly to help young adults (18-39) with cancer or recovering from it to share experiences and plan activities.
After treatment, you'll enter the Bridge to Next Steps Program. This program helps you and your child transition into post-therapy care.
At least two to three years after your child completes treatment, they can enter the Next Steps Clinic. This long-term follow-up program cares for cancer survivors. Our care team monitors for recurrence, manages late effects and promotes overall well-being.