A child was born limp and cyanotic at Ministry St. Joseph’s Children’s Hospital in Marshfield, Wisconsin. Aggressive bag-mask ventilation interrupted by repeated attempts at intubation resulted in abdominal distension and persistent desaturation prompting transfer to the operating room for a tracheostomy. However, no identifiable trachea was found.
The patient had tracheal agenesis, a rare anomaly occurring in fewer than 1 in 50,000 live births, with fewer than 200 births described in the literature.
 The surgical team at Marshfield consulted with the trachea surgical team at Children’s Wisconsin. They advised a laparotomy and a preemptive gastrostomy tube followed by a temporary clip at the gastroesophageal (GE) junction in an effort to avoid further compromise of ventilation from increasing gastric distension.
The surgical team at Marshfield consulted with the trachea surgical team at Children’s Wisconsin. They advised a laparotomy and a preemptive gastrostomy tube followed by a temporary clip at the gastroesophageal (GE) junction in an effort to avoid further compromise of ventilation from increasing gastric distension.
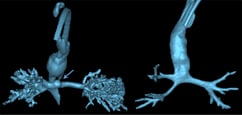
The patient was then transferred to Children’s, where a CT angiogram confirmed long-segment tracheal agenesis with an esophageal fistula at the level of the carina, and distal bronchomalacia. A chest x-ray evaluation showed rib fusion anomalies, and an echocardiogram revealed a large patent ductus arteriosus (PDA).
At 4 days old, a video laryngoscopy showed a definitive division of the esophagus distal to the fistula. So surgeons performed the first of what would be five surgeries, stapling the gastrointestinal junction below the level of the esophageal fistula and ligating the PDA.
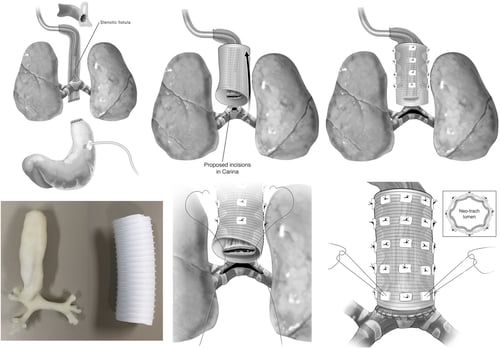
Over the next three months, the patient underwent additional surgeries to construct an esophagus. This included the creation of a “pseudo” tracheostomy, which was replaced a few weeks later with a custom 4.0 cuffed Bivona tracheal tube. At 3 months, surgeons performed an esophagocarinal fistula resection and external stenting of the “pseudo” trachea while the patient was on cardiopulmonary bypass. He was discharged home at 4 months, becoming the first patient with tracheal agenesis in the United States to survive to hospital discharge.
Later, the team reconnected the patient’s mouth to their stomach, allowing them to eat food for the first time.
Five years later, the child is doing very well with their neotrachea. “They are breathing without a tracheostomy, but eventually we will need to replace their neotrachea,” Dr. Mitchell says.
The team recently completed surgery in a similar case with an even smaller child. “Innovation comes out of necessity,” Dr. Mitchell says.
Below is the process of placing a custom 4.0 cuffed Bivona tracheal tube. Click to enlarge.
- Densmore JC, Oldham KT, Dominguez KM, Berdan ER, McCormick ME, Beste DJ, et al. Neonatal esophageal trachealization and esophagocarinoplasty in the treatment of flow-limited Floyd II tracheal agenesis. J Thorac Cardiovasc Surg. 2017;153(6):e121-e125.