Our team gives you and your family the best and safest care possible. We provide a comfortable and welcoming environment during every step of your journey. We’re here for you, from initial diagnosis to long-term management.
Deciding where to seek treatment for your child's GI issues can be difficult and stressful. The range of options, including new and experimental treatments, can be hard to figure out. We want to make it as easy as we can.
In addition to world-class care, we provide many resources for kids and their families. We want your journey to be as smooth as possible, given the difficult circumstances.
Before
For your first visit to the IBD Program, we may ask for:
- Your child’s medical history
- Past test results
- List of medicines
- Reports from previous procedures
If you have any questions before our first meeting, please contact our team.
During
Your care team creates a welcoming, familiar, healing place for your family. We know that each child with a gastrointestinal disease like Crohn’s needs a unique care plan. We will work with you to figure out the best care options for your child.
Our IBD care team includes:
- A pediatric gastroenterologist and expert in IBD. They’ve seen many difficult and unusual cases.
- A pediatric nursing staff with knowledge of Crohn’s disease and care.
- A registered pediatric dietician who manages your child’s diet and nutrition while considering the impact on their Crohn's disease.
- An IBD psychologist who focuses on kids with inflammatory bowel disease and other chronic diseases.
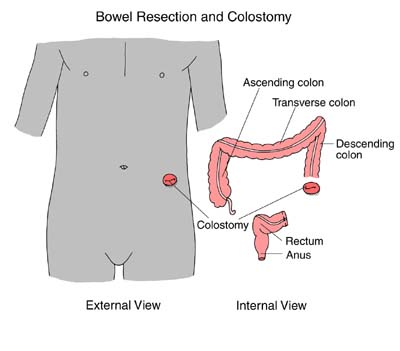
- Pediatric surgeons who are experts in complex IBD surgery, including less invasive methods such as robotic surgery.
- Social workers who can assist with the financial challenges of care.
Depending on your care plan, we may work with other highly skilled experts across Children’s Wisconsin. We take great pride in giving your child the very best care.
After
Care for Crohn's disease is lifelong. It requires long-term medical care.
The goal is to keep your child in remission which means that the disease is not active and symptoms go away. Remission is aimed to last for months or even years. There is no way to predict when remission may occur or when symptoms will return. However, in Crohn's disease, symptoms often come back and changes may be needed to control disease or symptoms.
Our team is here to monitor your child, help during flare-ups, consideration of offer new medicines and treatments when they become available and provide long-term care for your whole family. You can always contact our team if you have any questions.