At 2:50 p.m. on Nov. 20, 2020, pagers started beeping throughout Children’s Wisconsin. Mass casualty incident, prepare for a surge of patients. Physicians, surgeons, nurses, social workers, therapists and technologists hurried to the Emergency Department and Trauma Center, and waited.
On the news, law enforcement and first responders converged on Mayfair Mall less than 3 miles away and victims were seen being loaded into ambulances. Everyone would later learn that a 15-year-old opened fire at the mall, sending eight people to local hospitals.
One patient was treated from the incident by the Emergency Department and Trauma Center at Children’s Wisconsin. In fact, that child was the only victim from a mass shooting the team at Children’s Wisconsin treated in all of 2020. However, they did treat 79 victims who sustained gunshot wounds in 2020 in isolated incidents. 79 children with gunshot wounds. More than double the kids they saw in 2019 — 38.
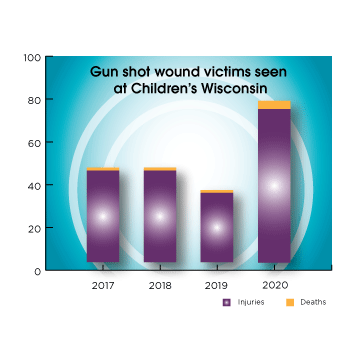
Six of those children didn’t survive. The team at Children’s Wisconsin has never treated that many deaths from gunshot wounds in one year, even though, in fact, guns are the second-leading cause of death for Wisconsin children ages 1–17i. Sadly, the number of kids who don’t survive is even higher than what the clinical teams at Children’s Wisconsin cares for, as some kids never make it to the hospital in time. According to the Milwaukee Homicide Review Commission, 27 kids under the age of 17 died from homicide in 2020.
The number of children impacted goes well beyond those who die from gun violence. While the clinical team at the hospital treated only one patient from mass shootings in 2020, the Community Health team at Children’s Wisconsin worked with families from more mass shootings in Wisconsin and 201 homicides that year. Even when children aren’t physically injured by an event like a mass shooting, they’re impacted emotionally and psychologically. That’s when the Community Health team, made up of crime victim advocates, community navigators, nurses and therapists, is dispatched to help families stabilize after a traumatic event and begin the recovery process.
This type of violence isn’t just a single moment or act, it’s a disease — an epidemic. The impact of gun violence on children has ripple effects that extend far beyond those injured or killed — the families and friends of victims, the children who watched as someone was shot, the generations of people who are stigmatized because of gun violence, the teams who see it every day at work…the list goes on.
This is the first in a series of blog posts that will share pieces of the puzzle of violence. A puzzle with many pieces, violence doesn’t have one perspective or solution, but instead is a complex issue that will require many people and a lot of work to combat. The series will explore different perspectives of individuals who respond to the call to serve victims and are impacted by violence, and different interventions to help break the cycle of violence. The goal for everyone is to prevent another record year of children being harmed.
Treating the wound: Emergency and trauma teams at Children’s Wisconsin
A resuscitative or emergency department thoracotomy (EDT) is performed in only the most extreme situations. The goal: Get the patient’s heart pumping again. If a patient comes into the Emergency Department with blood loss due to a penetrating injury (most often a gunshot wound) and their heart has stopped, the team has 60 seconds to perform an EDT. The clock starts as soon as the patient enters the Emergency Department.
Open the chest with a horizontal incision from the sternum to the back, separate ribs: 20 seconds
Clamp aorta to stop blood flow to lower body and preserve blood for brain and heart: 20 seconds
Place hand on heart and massage as a form of CPR: 20 seconds
While this may sound like something commonly seen on shows like Grey’s Anatomy, most pediatric surgeons never have to perform one. David Gourlay, MD, medical director of trauma at Children's Wisconsin and professor and chief of surgery at the Medical College of Wisconsin, says EDTs are something you train for, but hope you never have to do. The Trauma team at Children’s Wisconsin had to perform two EDTs on kids in 2020…in one week.
“A trauma room is usually pretty full with about 20 people working together quickly to save a child’s life. When we have to perform EDTs, it can be shocking to those in the room who don’t spend most days in surgeries,” said Dr. Gourlay. “It’s a heroic procedure that has to happen extremely quickly. The fact that we had to perform two in 2020 is an indication of how severely gun violence impacted our community last year.”
It was late April when Dr. Gourlay recognized 2020 was going to be different.
“We’re used to seeing an increase in patients coming to the Emergency Department as soon as summer begins because of accidents that happen with kids being outside more — things like falls, bike accidents, etc.,” said Dr. Gourlay. “But in April, we saw a drastic increase in gunshot wound patients.”
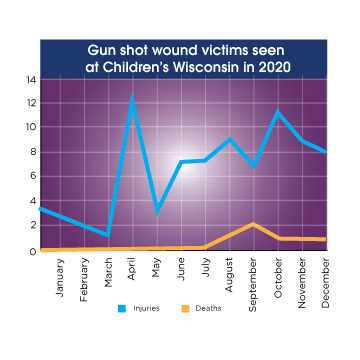
The team treated one gunshot wound victim in March, but then treated 12 in April. Over the next five months, the team treated the same number of victims as the entirety of 2019. While there hasn’t been any data to pinpoint why the rise in gun violence happened starting in April, it’s easy to connect the dots to the COVID-19 pandemic. Mid-March, schools in Wisconsin announced closures to help mitigate the spread of COVID-19, meaning the increase in victims aligns with when kids were home much more.
“Our teams are dedicated to not only treating the patients who come to us with gunshot wounds, but also helping prevent them from coming to see us in the Emergency Department in the first place and mental health is a huge piece of that,” said Dr. Gourlay. “2020 only highlighted the need for preventative care related to mental and behavioral health.”
Beyond the wound: A mental health crisis contributing to gun violence
Children, families and communities who experience violence also experience trauma. Trauma isn’t just physical. It’s emotional, psychological, behavioral — and cyclical. Children who are exposed to violence are more likely to develop mental and behavioral problems, and in the worst cases, this can lead them to resort to violence as well.
“The issue of violence increasing in our area is complicated and one in which we are committed to resolving. One aspect we can clearly see and address is mental and behavioral health,” said Smriti Khare, MD, president of Children’s Wisconsin Primary Care. “We put a focus on mental and behavioral health in the past year and are pushing for solutions as quickly as possible.”
The commitment of Children’s Wisconsin to mental and behavioral health is one piece of the puzzle, helping support children and families in coping with and preventing violence. In 2020, Children’s Wisconsin made a $150 million commitment and plan to detect mental health needs sooner, improve access to services and reduce the stigma around the illness. To support that work, Children’s Wisconsin also:
- Received the largest single donation in its history with an anonymous donor pledging a $15 million match for donations to Children’s Wisconsin that are designated to support mental and behavioral health services.
- Established a crisis response team in the Emergency Department, available 24 hours a day, seven days a week for children with mental and behavioral health needs thanks to a grant from the United Health Foundation.
- Launched Shine Through, an awareness campaign to help address the mental and behavioral health challenges of kids.
- Announced a partnership with Milwaukee County and the three other Milwaukee health systems to build and operate a new mental health emergency center.
Throughout Children’s Wisconsin, there are doctors, administrators, staff, fundraisers and others who understand it is not enough to be exceedingly good at treating the immediate result of the violence — the physical wound. That is just a small sliver of that child’s whole experience with violence. It’s our vision for Wisconsin’s kids to be the healthiest in the nation, and to reach that goal we must help keep kids protected from violence in the first place.
In the upcoming second blog post in this series, we’ll look beyond the doors of the Emergency Department at Children’s Wisconsin and share how the community is impacted by violence, and how we can start addressing it.
i Source: Giffords Law Center, US Bureau of Economic Analysis, CDC WISQARS, World Bank
The Milwaukee Neighborhood News Service put together a list of resources to help keep kids safe and engaged. You can see the full list on their website.







