In this section
What is intussusception?
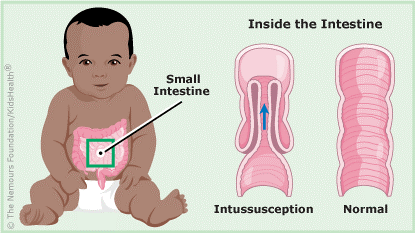 Intussusception happens when one part of the bowel slides (telescopes) into another part. This causes the bowel to be blocked (obstructed). It happens more in boys than girls.
Intussusception happens when one part of the bowel slides (telescopes) into another part. This causes the bowel to be blocked (obstructed). It happens more in boys than girls.
What are the different types of intussusception?
- Idiopathic. The cause is not known. It often happens after a viral illness in children ages 6 months to 2 years old.
- Lead point. This is due to an abnormality of the intestine, such as a lymph node or polyp. Most often it happens in older children.
- Post-operative. This can happen after a child has surgery on the chest or abdomen.
What are the signs/symptoms?
Your child may:
- Not act right.
- Have belly pain that makes them scream and pull their legs up to their chest. The pain normally lasts for about 3 to 5 minutes. The pain goes away for 20 minutes to 2 hours and then comes back. When the pain is gone your child will probably stop crying and rest. This cycle normally repeats itself.
- Vomit. Sometimes it may be green or yellow.
- Have a low-grade fever.
- Have a bowel movement (poop) that looks like currant jelly. This means it may be dark, bloody, or jellylike.
- Become more sluggish and tired as the illness progresses.
When should I call the doctor?
Intussusception is a medical emergency. Call your doctor or get emergency medical help right away if your child has any symptoms of intussusception, such as:
- repeated crampy belly pain
- vomiting
- drowsiness
- passing of currant jelly stool
Most infants treated within the first 24 hours recover completely with no problems. But untreated intussusception can cause serious problems that get worse quickly. So it's important to get help right away — every second counts.
What tests will be done?
- You will be asked about your child’s symptoms. The symptoms help the doctor diagnose the problem.
- The doctor will do an exam. The doctor will try to feel for the area of intestine that has “telescoped” into itself. This may feel like a sausage-like mass.
- An x-ray of your child’s belly may be done. The x-ray may show an obstruction.
- An Ultrasound is often performed to confirm the diagnosis.
- A barium or air enema may be done. This can diagnose and sometimes cure the problem. A radiologist puts a tube into your child’s rectum. Air or barium is then put into the intestines to show the position of the intestines. If the intestines have “telescoped”, this test may push the intestines back into their normal position.
How is it treated?
If an enema does not cure the problem, a second enema may be used. Sometimes, the enema does not cure the intussusception. Then, surgery is needed.
What care will my child need if the enema works?
Your child will likely go home. If your child does have to stay in the hospital:
- A nurse will check your child’s temperature, heart rate, breathing and blood pressure.
- Your child will be able to try to drink clear liquids (juice, soft drinks, Jell-O®, Popsicles®). Once your child handles clear liquids, eating regular food will be allowed. It is important to tell the nurse if your child vomits.
- Save any bowel movements (poop) in the toilet or diaper for the nurse to see. If your child does well with regular food or formula, you will be able to take your child home.
How will my child be prepared for surgery?
- An IV (intravenous tube) put into a vein in your child’s hand or foot. The IV will give your child fluids. These fluids will keep your child from getting dehydrated.
- A doctor or nurse may put a tube, called a nasogastric or NG tube, down your child’s nose and into the stomach. This tube will drain the stomach. The drainage may be clear, brown, yellow or green.
- IV antibiotics may be given to keep your child from getting an infection.
What will happen during surgery?
- Your child will need to have general anesthesia for the surgery.
- Surgery is often performed either by a laparoscopic or open approach. The laparoscopic approach involves making 3-4 small (<1cm) incisions in the stomach area through which we can place a camera (laparoscope) and small instruments to reduce the intussuscepted bowel. The intestines will gently be “squeezed” back (un-telescope) into place.
- In some patients, the laparoscopic surgery is not possible to reduce the intussusception often because the intestine is irreversibly injured, or the surgeon identifies an abnormality that caused the intussusception. A small part of the intestine may need to be removed and the surgeon may make a small incision in order to remove a small piece of intestine and put it back together. The appendix may also be removed at the time of surgery.
- In very severe cases, part of the intestine may need to be brought out onto your child’s abdomen. This gives the rest of the intestine a chance to heal. Your child’s bowel movements will empty into a special bag worn on the abdomen. After a few months, your child will most likely have a surgery to put the intestine back together again. Your child can then have normal bowel movements.
What care will my child need after surgery?
- Your child will be given pain medicine after surgery to keep them comfortable.
- Your child will be asked to take deep breaths, cough and sit in a chair.
- Your child will be helped to walk after surgery. This helps prevent pneumonia. Babies may be held.
- A urinary catheter (tube) may be put in your child’s bladder during surgery to empty urine. Your child may also need this tube after surgery.
- Your child may not be able to drink anything right after surgery. An IV will still be needed to give fluids.
- The NG tube may be needed to empty your child’s stomach. It will be removed when your child’s stomach starts to growl and your child starts to pass gas. The doctors will tell you when your child can then drink and eat.
What will I need to do at home?
If your child had an idiopathic intussusception (cause not known) that was cured by a barium or air contrast enema:
- Follow any diet instructions given to you.
- Check your child’s bowel movements for several days. At first, your child’s bowel movements may be full of a white or chalky substance (if you child had a barium enema).
- It is very important to watch for signs of intussusception. Tell the doctor if your child has any abdominal pain, vomiting, dark or bloody stools. Sometimes intussusception occurs again.
If your child had an operation to cure the intussusception:
- Follow any diet instructions that you were given.
- Check that your child is having regular bowel movements.
- Care for the incision as you were instructed.
- Have your child take a bath or shower when the doctor tells you this is okay to do.
- Watch for any signs of infection. Signs include redness, swelling, or drainage at the incision or fever over 101.2° F (38° C).
- It is also important to watch for signs of intussusception. Tell the doctor if your child has any abdominal pain, vomiting, dark or bloody stools. Sometimes intussusception happens again.
- Give your child medicine for pain as needed.
- You do not need to limit your child’s activity. Infants and toddlers normally limit themselves and get more active as they are able.
- Keep the follow-up appointment with your child’s surgeon. This appointment is usually one month after your child goes home.
ALERT: Call your child’s doctor, nurse, or clinic if you have any questions or concerns or if your child has special health care needs that were not covered by this information.
This webpage was created to help you care for your child or family member. It does not take the place of medical care. Talk with your healthcare provider for diagnosis, treatment and follow-up.
Wisconsin's highest-rated pediatric surgical center
Recognized by the American College of Surgeons, our Level I verification represents the highest level of recognition for hospitals that perform complex surgical procedures in newborns and children.
Make an appointment
To make an appointment, call our Central Scheduling team or request an appointment online.
