
A Better Way: How a New Technique Is Improving Care for Kids With Chronic GI Issues
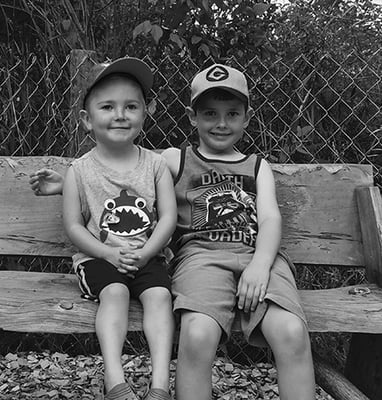
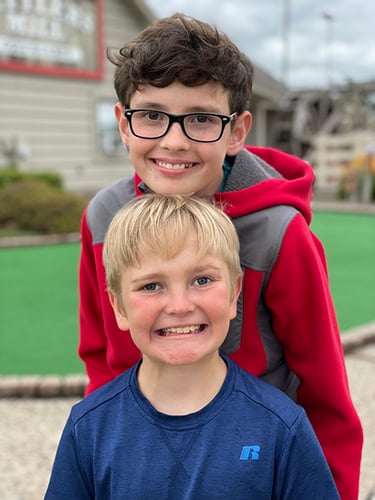
Owen and Ean may be brothers, but they’re quite different. Owen, 16, enjoys biking, drawing and playing the piano. While Ean, 13, plays basketball whenever he can, likes Legos and has a black belt in karate. But one thing they have in common is living with a chronic disease called eosinophilic esophagitis, also known as EoE.
Owen’s journey began when he was just a few weeks old and started experiencing eczema while nursing. Then, at 6 months old, when children are often introduced to solid foods, his mom, Ann, fed him some yogurt. Owen broke out into hives. This led her to seek a local allergist in their hometown of Oshkosh, Wisconsin.
 At the time, Ann was told Owen’s reaction wasn’t necessarily an allergy nor an uncommon occurrence. She was advised to wait a few weeks and then feed him yogurt again. But each time she did so, as instructed, his reaction got progressively worse. Owen had the same reaction to eggs. Only after the second attempt, he had to be rushed to the emergency department at their local hospital because his reaction was so severe.
At the time, Ann was told Owen’s reaction wasn’t necessarily an allergy nor an uncommon occurrence. She was advised to wait a few weeks and then feed him yogurt again. But each time she did so, as instructed, his reaction got progressively worse. Owen had the same reaction to eggs. Only after the second attempt, he had to be rushed to the emergency department at their local hospital because his reaction was so severe.
Before his 1st birthday, Owen was diagnosed with allergies to peanuts, tree nuts, dairy and eggs. He also needed to avoid wheat and soy. Because Ann was still nursing, she began to avoid these foods as well. She also started seeing a local nutritionist who she hoped would advise her on what to eat to ensure Owen got the nutrients he needed to grow and thrive.
“I saw a local nutritionist who gave me a bunch of information,” said Ann. “But most of the allergen-free options she discussed were highly processed. This was my first child, and I was much more aware of what I put into his body and mine. So, I really didn't know what to feed him. I just felt like I needed more resources.”
As Ann struggled to find the support she so desperately needed, her sister suggested taking Owen to Children’s Wisconsin. While it was nearly two hours from their home, she was eager to find answers and help her son.
“And that’s how we ended up at Children’s Wisconsin,” said Ann.
Reaching a diagnosis and a path forward
 Once established with an allergist at Children’s Wisconsin, Ann began to feel a sense of relief and support she hadn’t felt prior. Owen’s new allergist also recommended they see a nutritionist at Children’s Wisconsin. Given their food limitations, she felt this was essential in ensuring Ann had the resources and guidance on nutritious food options.
Once established with an allergist at Children’s Wisconsin, Ann began to feel a sense of relief and support she hadn’t felt prior. Owen’s new allergist also recommended they see a nutritionist at Children’s Wisconsin. Given their food limitations, she felt this was essential in ensuring Ann had the resources and guidance on nutritious food options.
“I’ll always remember her because she was so helpful,” Ann said about Owen’s nutritionist, who ultimately led her down the path to a diagnosis.
At that first appointment, she told the nutritionist that Owen also seemed to struggle swallowing. “I told her that Owen occasionally would swallow hard. And that something appeared off in the way he swallowed,” she said.
Ann had previously discussed Owen’s swallowing challenges with his local pediatrician but was told that babies sometimes struggle to manage their saliva. The nutritionist, however, immediately recognized that this was common in children with eosinophilic esophagitis (EoE), a condition that causes an abnormal immune response to certain foods, leading to swelling in the throat, dysphagia (difficulty swallowing), vomiting and abdominal pain.
She referred Owen to one of her colleagues in the Children’s Wisconsin Gastroenterology, Liver and Nutrition Program. At just 15 months old, Owen underwent his first sedated upper endoscopy, a procedure that involves inserting a soft, flexible tube with a camera and light into the mouth. It allows doctors to examine the esophagus (a tube that connects the throat to the stomach) down to the stomach and small intestine.
Before the procedure, Owen was started on an IV and sedation using general anesthesia to ensure he was asleep for the procedure. During the exam, tissue samples, known as biopsies, were taken. The biopsies were then examined under a microscope, and it was confirmed that Owen had EoE.
While doctors don’t yet know what causes the abnormal immune response in people with EoE, it’s believed there may be a genetic predisposition. Children with family members who have allergic conditions such as asthma, hay fever, food/seasonal allergies and eczema may be at higher risk of developing EoE. It affects nearly 1 in 10,000 children and is more common among school-age children and boys. Treatment typically includes a food elimination plan, dietary changes and medication to reduce inflammation.
A couple of years after Owen’s diagnosis, his brother Ean was born. By about 4 months old, Ean began facing similar challenges, though with different symptoms. Ean's challenges included poor growth, acid reflux and some food sensitivities. Ean was eventually diagnosed with EoE. The boys’ diagnoses also led to Ann’s eventual diagnosis.
The challenges of managing a chronic disease
 Since being diagnosed with EoE, both boys have undergone many sedated upper endoscopies to manage and monitor their condition and ensure their current treatments are working. They are on different treatment plans because what works for one child does not always work for another.
Since being diagnosed with EoE, both boys have undergone many sedated upper endoscopies to manage and monitor their condition and ensure their current treatments are working. They are on different treatment plans because what works for one child does not always work for another.
“When EoE is not well-controlled with one medication, we try a different medication. But every time we try a different medication, we have to follow up with a scope to make sure that medication is working,” said Rose Lee, MD, a pediatric gastroenterologist at Children's Wisconsin. “Until we find a medication that works for the patient, the kids typically get scoped every three to four months. But once we find a medication that works and we know the disease is in remission, we do a surveillance scope every two to three years.”
A sedated upper endoscopy requires that a child fast for eight hours before the procedure. They need to arrive approximately two hours early to prepare for an IV and general anesthesia. The recovery time typically lasts an hour or more. And they can’t resume normal activities for the remainder of the day.
Every time the boys were due for their next endoscopy, it would take up their entire day. And as they got older, this became more disruptive. They’d miss a full day of school and extracurricular activities due to the preparation, travel and recovery time.
"You take this bad medicine, and then you go to sleep, and your whole day would be ruined because you have to go under,” said Owen. “Then you can't really go back to activities or school.”
This was their norm for many years. That is, until 2022.
A better way to scope
 In 2022, the Gastroenterology, Liver and Nutrition Program at Children’s Wisconsin began offering a less invasive procedure called an unsedated transnasal endoscopy (TNE). This niche procedure uses a very thin, flexible scope inserted through the nose to examine the esophagus, stomach and intestines. TNE has many uses, one of which is diagnosing EoE in children.
In 2022, the Gastroenterology, Liver and Nutrition Program at Children’s Wisconsin began offering a less invasive procedure called an unsedated transnasal endoscopy (TNE). This niche procedure uses a very thin, flexible scope inserted through the nose to examine the esophagus, stomach and intestines. TNE has many uses, one of which is diagnosing EoE in children.
One major advantage of TNE is that it does not require anesthesia or sedation — it’s performed with only a mild numbing agent. This makes the procedure faster than a sedated upper endoscopy, resulting in a quicker recovery time of about five to 10 minutes. Additionally, no IV is needed, and the child only needs to fast for two to four hours before the procedure, as opposed to eight hours for a sedated upper endoscopy.
“For sedated upper endoscopy, kids go through general anesthesia. They typically are pretty groggy, and some kids have nausea from the general anesthesia. So, they can’t really go back to school or sports. They have to take it easy for the rest of the day,” said Dr. Lee, who is also an assistant professor of gastroenterology at the Medical College of Wisconsin, the academic partner of Children’s Wisconsin. “With TNE, we don’t use general anesthesia, so they can actually go back to school and do their daily activities right away.”
Katherine Vaidy, MD, a pediatric gastroenterologist at Children's Wisconsin, stressed the importance of not just having the parents on board for the procedure but the children as well.
“I didn't know at first if I wanted to or not,” Ean said about undergoing the unsedated TNE procedure. “Then I just decided to try it once. I did it twice now, and I probably will do it next time, again.” He added that while he had to sit still during the procedure, he got to watch a show of his choosing — “Phineas and Furb.” “You get to wear these little goggles,” he added.
Owen said the first time he did the TNE procedure, he was a bit scared and had some discomfort. But the second time around was much better.
“It just feels really weird because you can't swallow,” he said. “The second time, I felt a little better. They put water in the scope, and it felt soothing to make it more relaxing.” He concluded that the TNE procedure was better than the sedated upper endoscopy. “You don’t have to have your whole day ruined. You can just go back to your day because it takes all of five minutes versus the other one that takes all day.”
Ann added that it’s wonderful not to have to put the boys through anesthesia — and that any time you can avoid that, all the better. “It's a necessary procedure. So, the less invasive, the better, especially when we have to do it more than once a year, every year.”
Anesthesia is generally very safe, and most kids don’t have problems with it. However, minimizing frequent or prolonged use of anesthesia is typically preferred as children's brains continue to develop throughout childhood. In some cases, though, anesthesia is medically necessary, particularly among very young children, during surgeries or when a child has a severe developmental delay or medical condition.
A commitment to continuous improvement
 As of 2024, more than 30 centers across the country offer the TNE procedure. However, fewer than 10 centers can perform a full endoscopy using this technique.
As of 2024, more than 30 centers across the country offer the TNE procedure. However, fewer than 10 centers can perform a full endoscopy using this technique.
Over the past two years, the criteria for TNE through the Gastroenterology, Liver and Nutrition Program at Children’s Wisconsin have expanded considerably. Kids with esophageal symptoms like dysphasia or even abdominal pain, those who may have celiac disease or who typically need a sedated upper endoscopy are now offered the TNE procedure as well.
Dr. Lee added that her team is dedicated to continuous improvement in how they perform procedures like TNE. They’re committed to conducting research and listening to feedback from patients like Owen and Ean to make these procedures more comfortable and an overall better experience.
“Children's Wisconsin has tweaked the procedure to make it far more comfortable. Nobody says, ‘Oh, it's great, and let's just do it for fun.’ But it was much more tolerable the second time around,” said Ann. “The boys are much more open to doing it solely that way instead of going back to the old way.”
The shift to TNE has not only reduced the physical strain on the boys, it has also been a massive relief for their family. They no longer have to endure the anxiety and exhaustion that comes with sedated upper endoscopies. Instead, they can focus on the boys' well-being and day-to-day activities. The ability to return to school and everyday life right after the procedure has been a significant benefit.
“The numbing goes away after five minutes, and they get to go out to lunch and go back to school,” said Ann. “It’s easier to get the kids on board when they know it's not going to take up the whole day.”
Children's Wisconsin Resources

Written by
Erin Kohlmann
Writer
Related Stories
No related articles found.



