When Derell was 8 years old, he had trouble staying focused in school and following all the rules. He was repeatedly disciplined for fidgeting, tapping his pencil and talking out of turn. When he was finally suspended for disruptive behavior, Derell –– frustrated by the feeling that he couldn’t do anything right –– lashed out at his teacher.
His mom, Etta, was frustrated too. For a time, she was being called into school nearly every day because of Derell’s behavior issues. “If I didn’t come and help out, they were going to suspend him again,” she said.
Even worse, he was starting to show signs of depression as a result of his struggles at school and with his peers.
“Derell didn’t know how to talk through conflicts with other kids,” said Etta. Instead of having fun playing with friends, Derell was getting bullied, feeling excluded and coming home upset.
Etta is an experienced mother of three, but her two older children never had behavioral or emotional challenges like Derell’s. She sought help from a local doctor’s office and took Derell to therapy appointments. “The doctor filled out some forms and sent them to the school,” said Etta, “but there wasn’t much follow-up.” Therapy was also a disappointment. “The office was a dingy room in a basement, and the therapist didn’t connect with my son.” Derell often fought going to his appointments.
When Children’s Wisconsin opened the Midtown Clinic close to her home, Etta jumped at the chance to take her son there. Derell started seeing a Children’s Wisconsin pediatrician, and screenings showed that Derell’s challenges with attention and self-regulation were contributing to his problems. The team at the Midtown Clinic was called into action right away.
A novel approach to behavioral health
At the Midtown Clinic and three other neighborhood primary care clinics, Children’s Wisconsin is piloting the integrated behavioral health program, which brings behavioral health therapists and pediatric psychologists into the primary care setting. But it’s not just a co-location of offices –– behavioral health providers are integrated into every aspect of care, from informal conversations in the pediatrician’s office, to patient consults, to providing short-term treatment within the child’s regular medical care.
 “Pediatricians and behavioral health providers work together as a team to meet the needs of patients,” said Robert Rohloff, MD, director of quality and safety of primary care at Children’s Wisconsin. “Not only does this help patients access care quickly and conveniently, it also means our pediatricians are being trained in behavioral health, and are more confident and capable of handling these issues within the context of a regular doctor’s visit.”
“Pediatricians and behavioral health providers work together as a team to meet the needs of patients,” said Robert Rohloff, MD, director of quality and safety of primary care at Children’s Wisconsin. “Not only does this help patients access care quickly and conveniently, it also means our pediatricians are being trained in behavioral health, and are more confident and capable of handling these issues within the context of a regular doctor’s visit.”
What’s more, the pediatric residents and psychiatry residents who train at the Midtown Clinic are also learning from the model. “Residents may get one short rotation or even just a few hours of behavioral health training as part of their medical education,” said Nick Young, PhD, one of the two full-time pediatric psychologists at the Midtown Clinic. That lack of training is at odds with the growing crisis of child mental health. “Here at Midtown, our pediatricians and pediatricians-in-training are learning how to care for behavioral and mental health issues every day, through real clinical experiences.”
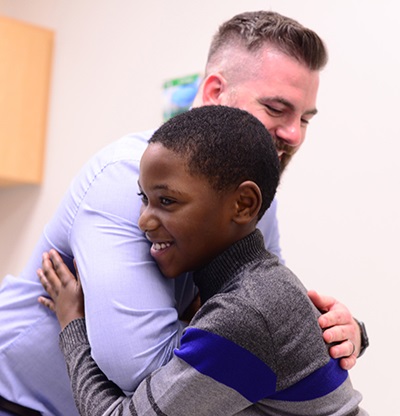
Dr. Young met Derell and his mom at a routine pediatrician visit, where he was introduced as a member of the care team in what doctors call a “warm handoff.” He offered some immediate short-term interventions and support with Derell’s pediatrician Colleen Maroney, MD, taking part in the conversation.
For Dr. Maroney, having the daily support of on-site pediatric psychologists is a gamechanger. Together, she and Dr. Young, along with Derell’s mom, developed a plan of care for Derell, which included individual appointments right down the hall in Dr. Young’s comfortable office.
When Derell was asked what he works on with Dr. Young, he stopped to think, then carefully counted out three things on his fingers. “How to be kind, staying focused, getting along at school and at home.” Then he turned to his mom and smiled.
Shifting attitudes, improving lives
The integrated behavioral health model helps patients and families shift their perception of mental health services. Making behavioral health a routine part of health care is tremendously helpful in normalizing it.
“In our culture, we’ve come a long way in our ability to talk about behavioral and mental health, but there are some invisible attitudes that inform our thinking,” said Dr. Young. “People equate getting treatment to having something wrong with them, and as humans we want to feel normal and accepted. Naturally, this may lead to resisting those services. Ultimately, it’s the pediatricians themselves, like Dr. Maroney, who help normalize it.”
Once he was receiving the right care, Derell’s behavior transformed rapidly. By the end of second grade, his grades had improved and he was getting along with other kids. Now, as a third-grader, Derell is on top of the world. When asked if he has friends at school, Derell grinned and said, “Yes, plenty.” He also has a favorite subject –– math. And he thinks he might like to be a school principal someday.
For Etta, the team approach to her son’s care has made all the difference. “I feel they really want to help us,” she said. “And everything is all in one place –– the doctors work together and Derell even goes to the dentist here.” Derell actually gets excited when he comes to Midtown Clinic.
“I love this place,” said Derell. “It’s like a second home to me.”
Dr. Young and his counterpart, Brittany Mathews, PhD, provide short-term treatment for kids. “Eight sessions is generally our limit,” said Dr. Young. “If kids need more intensive therapy, we refer them to community providers, just as we would refer for any other type of specialty care like orthopedics or asthma care.”
That’s not to say Dr. Young and Dr. Mathews don’t stay involved with their patients. Over the years, they will continue to play a part in kids’ healthy growth and development. That might mean stepping into an annual checkup to talk with a family about managing temper tantrums, consulting with teens about emotional changes during adolescence, or sharing strategies to make healthier choices about diet and exercise.
Last September, when Derell was in a bus accident and hit his head, Dr. Young and Dr. Maroney worked together to respond to his symptoms, which included behavioral symptoms. “Because Dr. Young had background on Derell’s behavioral issues, we were able to immediately refer him for the appropriate follow-up care, which included an MRI,” said Dr. Maroney. “Without a behavioral expert on Derell’s team, who knew him and his background, it could have potentially taken us longer to identify the right care in a timely way.”
“What’s powerful about this model is that we’re catching many more potential issues much sooner, and serving a greater number of families, so our impact is greater,” said Dr. Young. The potential to improve the community’s health is huge.
Families more engaged
Not only is integrated behavioral health providing more care sooner to families, but data from the Midtown Clinic shows that families who meet and talk with behavioral health specialists during a primary care appointment are more likely to get and stay involved in their child’s care. Participating families have 85 percent fewer no-shows or cancellations for primary care appointments, and they follow up with behavioral health specialists on average 16 days faster than families not served by integrated behavioral health providers.
“By building trust and relationships from early on, families are more invested in their child’s care and more comfortable. This means more follow-through, and ultimately better health outcomes for kids,” said Dr. Young.
It also means a positive impact on the entire healthcare system, by reducing emergency department visits and health crises, and making care more efficient though better attendance and follow-up in primary care.
Philanthropic support
Donor support has made possible the two-year pilot of the integrated behavioral health program at the Midtown Clinic and several neighboring clinics, where behavioral health providers completed more than 1,000 patient visits between October 2017 and September 2018. With continued philanthropic support, plans to expand integrated behavioral health to other Children’s Wisconsin primary care offices in southeast Wisconsin are underway.
 “We know that every population has challenges with mental and behavioral health, and every population can benefit from this approach,” said Dr. Rohloff. “We are excited to be on the cutting edge of this care that we believe can truly revolutionize how we think about not only mental and behavioral health, but the overall health of children and families.”
“We know that every population has challenges with mental and behavioral health, and every population can benefit from this approach,” said Dr. Rohloff. “We are excited to be on the cutting edge of this care that we believe can truly revolutionize how we think about not only mental and behavioral health, but the overall health of children and families.”
While Dr. Young and Dr. Mathews will continue to support kids and families by providing critical interventions, the ultimate goal of integrated behavioral health is to empower pediatricians to become more comfortable supporting the mental health of their patients. “We are already seeing increased expertise in our pediatrician partners as they provide behavioral health guidance to patients and families,” said Dr. Young.
For Derell, having Dr. Young in his corner has meant the world. As he heads out of the clinic and home with his mom, he and Dr. Young do their special multi-part handshake, laughing when they can’t quite remember all the steps. Then they share a hug, smile and wave goodbye.







