
How a surgeon at Children’s Wisconsin is looking to change the way we treat appendicitis
On a late Sunday afternoon in early August, after a long, hot weekend of playing and swimming and running around, 10-year-old Henry Copps came home for dinner complaining of a stomach ache.
As active kids of that age are prone to the occasional stomach ache, Henry’s mother, Julie, didn’t think much of it. Henry poked at his dinner a bit and then went to bed.
But the next morning the stomach pain had worsened. Clutching a pillow to his stomach, Henry was unable to stand up straight.
Julie called Henry’s pediatrician and made an appointment for later that morning. The pediatrician told them he was quite certain it was his appendix and directed them to immediately go to the Emergency Department at Children’s Wisconsin.
“We were only there for about five minutes and the ER docs agreed with the pediatrician’s suspicion and sent him for an ultrasound, which confirmed the appendicitis,” said Julie. “When we heard that, my husband and I both thought, ‘Okay, he’s going to have surgery.’”
And if they had gone to pretty much any other hospital, he would have.
Since the appendectomy — the surgical removal of the appendix — was first introduced and mastered in the late 19th century, surgery has been the standard treatment for appendicitis. But one pediatric surgeon at Children’s Wisconsin is looking to change that.
For the past year, Dave Lal, MD, a pediatric surgeon at Children’s Wisconsin, has been participating in a national clinical trial testing non-surgical treatment for early appendicitis. The two-year trial was launched in 2016 with a $2.6 million grant from the Patient-Centered Outcomes Research Institute (PCORI) and includes 11 sites across the United States and more than 600 kids.
For the trial, when a child comes to the hospital and is diagnosed with early appendicitis, they are given a 24-hour course of IV antibiotics. During this time they’re closely monitored to make sure they don’t get sicker. If certain things happen — fever develops, heart rate increases — the patient has “failed” and they’re taken to surgery. If they improve, however, the child is sent home with a seven day course of oral antibiotics.
“We really want medicine to be more patient focused and more patient centered,” Dr. Lal said. “We provide families the information, including the risks and benefits, and we let them make that choice.”
Challenging more than a century of medical precedent has been met with the expected pushback, however.
“My wife is an adult surgeon and we have two boys. If our two boys had appendicitis and it was early, I would treat them with antibiotics. She would just take it out,” Dr. Lal said. “Even in our household we have different ideas. But the whole reason to do this trial is to answer that question. Is there some benefit in avoiding surgery and treating patients with antibiotics?”
At first, Julie and her husband, Andy, were skeptical.
“My initial thought was, ‘No, we’re not experimenting. It needs to come out,’” said Julie. “We know that when an appendix gets infected it comes out. That’s just the way it’s always been.”
And she’s not wrong. While the particulars of the procedure may have changed — from open to laparoscopic to single incision — the basic premise has remained for more than 120 years: surgically remove the infected appendix.
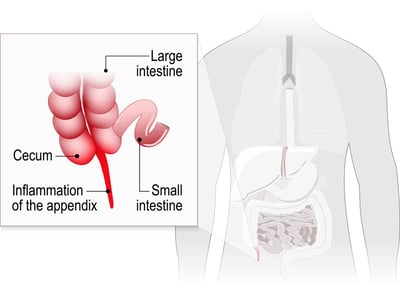
The appendix is a small sac located between the small and large intestine. During the first years of life, it functions as part of the immune system. But as children get older, the appendix ceases to function. At this point, the appendix is prone to irritation and infection — it often fills with mucus, stool or parasites. That’s appendicitis.
A ruptured appendix is so serious — life-threatening, in fact — because if it becomes perforated, all that infected material will leak into the abdomen and infect the surrounding organs. An irritated appendix can rapidly turn into an infected and ruptured appendix, sometimes within hours.
 The most common symptom of appendicitis is abdominal pain. This typically presents around the belly button or lower right side of the stomach and becomes worse over time. Breathing or coughing often intensifies the pain. Other symptoms include nausea and vomiting, loss of appetite, fever and chills, diarrhea or constipation and changes in behavior.
The most common symptom of appendicitis is abdominal pain. This typically presents around the belly button or lower right side of the stomach and becomes worse over time. Breathing or coughing often intensifies the pain. Other symptoms include nausea and vomiting, loss of appetite, fever and chills, diarrhea or constipation and changes in behavior.
Affecting approximately four in every 1,000 children under 14 years old, appendectomies are the most common emergency surgery in children. Despite how common the procedure is, however, no surgery is without risks. At Children’s Wisconsin, doctors believe there is no such thing as “routine surgery.” Any time a child is being put under anesthesia, there are inherent risks. That coupled with the decreased recovery time and cost makes non-surgical treatment an attractive option for many families.
While non-surgical management of appendicitis is not new, it has fallen out of favor in the last century or so. But Dr. Lal believes that advances in technology makes it worth revisiting.
“In the past, we didn’t have the technology to help us determine what is advanced appendicitis and what is early appendicitis,” said Dr. Lal. “Now with modern imaging we’re able to better discern who has really early appendicitis and would benefit from and be completely treated with antibiotics.”
After thinking it over for a while, Julie and Andy decided that if they could avoid surgery, it was worth a shot. For his part, Henry didn’t really care. He just wanted to feel better.
“Even though I’m a surgeon, obviously I want the best for my patients,” said Dr. Lal. “If there is a subset of patients who can get better and avoid surgery, I think that’s better for the patient and their families and we should offer that.”
 Henry started his course of antibiotics Monday evening and by the next day he was significantly better. He was discharged Tuesday evening and by Wednesday morning he was back to normal, spending the day swimming with a friend.
Henry started his course of antibiotics Monday evening and by the next day he was significantly better. He was discharged Tuesday evening and by Wednesday morning he was back to normal, spending the day swimming with a friend.
“It was amazing,” said Julie. “It was like he just had a case of strep throat or something.”
So far, Dr. Lal is seeing about a 20-30 percent failure rate.
“If you have 10 patients, two or three are not going to get better with antibiotics and will require surgery,” he said. “But if you look the other way, that’s 70-80 percent of patients who will do fine and never require an operation.”
Four months later, Henry continues to be part of that 70-80 percent of successes. He’s as active as ever — playing basketball and flag football and rock climbing — and hasn’t had any additional issues with his appendix.
Despite its success, though, there is one downside to the nonsurgical route, at least according to Henry.
“After he was feeling better,” Julie remembered, “Henry said the only reason he was sad he didn’t have the surgery is because he wanted to have a scar.”
Children's Wisconsin Resources

Written by
Evan Solochek
Writer
Related Stories
No related articles found.



