In this section
Ross Procedure
Provided by "Pediatric Heart Surgery — a reference for professionals"
Patient families can visit our Ross procedure page for more information and answers to common questions.
Pathophysiology
Aortic valve stenosis causes progressive left ventricular hypertrophy with associated sequelae of decreased ventricular function and myocardial ischemia. These factors place the patient at increased risk for sudden death. Aortic valve insufficiency results in left ventricular dilatation and decreased cardiac output. It can eventually lead to congestive heart failure. Exercise intolerance and exertional dyspnea can occur in patients with severe forms of aortic valve disease. The Ross procedure is an innovative technique that uses the patient’s own pulmonary valve for aortic valve replacement. A cryopreserved pulmonary valve homograft is used to replace the patient’s native pulmonary valve. The pulmonary autograft grows over time, making the Ross procedure an excellent choice for aortic valve replacement in infants and small children. Further, anticoagulation with warfarin is not required following the Ross procedure. In contrast to traditional mechanical aortic valve replacement, however, the Ross procedure is a more extensive operation. In addition, later replacement of the pulmonary valve homograft is generally required due to growth of the patient or degeneration of the homograft.
Surgical technique
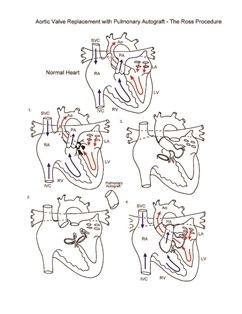
Aortic valve replacement requires cardiopulmonary bypass and aortic cross-clamping. The aorta is opened and the aortic valve is inspected. Once suitability for the Ross procedure has been determined, the pulmonary root autograft is excised. As the aortic root is excised, the coronary artery ostia are excised as buttons with adjacent aortic wall tissue. In children, implantation of the autograft is generally performed as a root replacement. The proximal pulmonary autograft is secured in the position of the native aortic root. The coronary arteries are next implanted, and the distal end of the autograft is anastomosed to the ascending aorta. A cryopreserved, valved pulmonary homograft is inserted in the position of the original pulmonary root. Transesophageal echocardiography is used to assess adequacy of the repair. Cardiopulmonary bypass time and aortic cross-clamp time required to complete repair are moderate to long.
Postoperative considerations
The postoperative course following the Ross aortic valve replacement procedure can be variable. This is an extensive operation, and inotropic support is frequently required. Invasive monitors used include arterial and central venous catheters. An LA line is used when needed for hemodynamic management. LA pressure acts as a surrogate for left ventricular end diastolic pressure, an excellent indicator of left ventricular performance. Non-invasive monitors include NIRS (near-infrared spectroscopy) probes to assess adequacy of regional and global perfusion and traditional pulse oximetry. Vasoactive agents might include epinephrine and/or milrinone. Numerous other agents are available and are tailored to the specific needs of the patient, targeting adequate oxygen delivery to the tissues of the body and optimization of cardiac output. Postoperative bleeding is a potential complication since there are numerous external cardiac suture lines exposed to systemic pressure. Cardiac arrhythmias occasionally occur following repair. Temporary atrioventricular pacing capability should be readily available. Postoperative intracardiac pressures should be normal. Slightly elevated left atrial pressure may occur secondary to left ventricular hypertrophy and poor left ventricular compliance. Arterial oxygen saturation should be normal. Length of hospital stay following the Ross procedure averages 5 to 7 days.
Physician consultation line
Staffed 24 hours a day.
- Refer a patient
- Discuss a case
- Arrange a transport
- Direct admission
(414) 266-2460
Toll-free: (800) 266-0366
Make a referral
Find helpful forms and phone numbers for making a referral to a specialty clinic at Children's Wisconsin.
Arrange a transport
A physician-led, clinical team is available 24 hours a day for transports to Children's from across the country.
Start Arranging Your Transport