In this section
Tricuspid atresia and single ventricle (Fontan Procedure and Glenn shunt Procedure)
Provided by "Pediatric Heart Surgery — a reference for professionals"
Patient families can visit our tricuspid atresia page, Glenn Procedure page or Fontan Procedure page for more information and answers to common questions.
Pathophysiology
The term single ventricle refers to any congenital cardiac anomaly in which one ventricle is hypoplastic or absent. Hypoplasia of either semilunar valve or either ventricular outflow tract is generally amenable to a biventricular repair. By contrast, significant hypoplasia of either atrioventricular valve or of the apical portion of either ventricle generally necessitates a single ventricle approach.
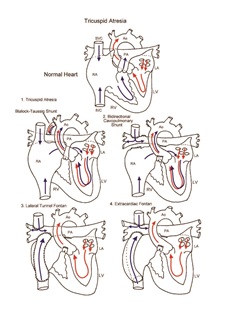
Tricuspid atresia is a form of single ventricle characterized by complete failure of development of the tricuspid valve. Incomplete development of the right ventricle and/or pulmonary artery is frequently associated. Systemic venous return to the right atrium must cross the atrial septum through an atrial septal defect and enter the left atrium to mix with pulmonary venous return. Obligatory mixture of systemic and pulmonary venous return results in systemic arterial oxygen desaturation. Prolonged systemic arterial desaturation can lead to progressive elevation of hematocrit and hyperviscosity. Late complications can result. Early diagnosis and management of single ventricle and its variants are essential.
Surgical technique
Initial efforts are directed at complete relief of systemic outflow tract obstruction and limitation of pulmonary blood flow to prevent development of elevated pulmonary vascular resistance. The ultimate goal is Fontan circulation, in which systemic venous return is directed to the pulmonary arteries without an intervening pumping chamber. Low pulmonary vascular resistance is essential for blood to flow to the pulmonary arteries passively at an acceptable venous pressure. Fontan circulation is usually accomplished in two stages. Initially, at 4 to 6 months of age, a bidirectional Glenn shunt is constructed to direct superior vena cava blood flow to the confluent pulmonary arteries. Fontan completion is accomplished by redirecting inferior vena cava blood flow to the pulmonary arteries with an intracardiac baffle or extracardiac conduit (see diagram). Fontan completion is usually undertaken at approximately 2 years of age.
Cardiopulmonary bypass is required for the Fontan completion procedure and is usually used for the cardiopulmonary shunt procedure as well. Use of aortic cross-clamping is variable and depends on the individual anatomy and surgeon preference.
Postoperative considerations
The postoperative course following the bidirectional Glenn shunt procedure is usually uncomplicated. The postoperative course following completion Fontan can be more complex. Invasive monitors used include arterial and central venous catheters. Atrial lines are used when needed for access and/ or hemodynamic management. Measurement of preload to the ventricle allows for titration of volume replacement and adjustment of vasoactive infusions. Non-invasive monitors include NIRS (near infrared spectroscopy) probes to assess adequacy of regional and global perfusion and traditional pulse oximetry. Vasoactive agents might include epinephrine and/ or milrinone. Numerous other agents are available and are tailored to the specific needs of the patient, targeting adequate oxygen delivery to the tissues of the body and optimization of cardiac output.
Special postoperative consideration is given to careFul monitoring of transpulmonary gradient (central venous pressure minus left atrial pressure). In addition to transpulmonary gradient, special attention is given to careful monitoring of central venous pressure as well as evidence of systemic venous congestion. Central venous pressure above 15–18 mmHg or transpulmonary gradient above 10 mmHg indicates difficulty with passive flow of blood across the
Physician consultation line
Staffed 24 hours a day.
- Refer a patient
- Discuss a case
- Arrange a transport
- Direct admission
(414) 266-2460
Toll-free: (800) 266-0366
Make a referral
Find helpful forms and phone numbers for making a referral to a specialty clinic at Children's Wisconsin.
Arrange a transport
A physician-led, clinical team is available 24 hours a day for transports to Children's from across the country.
Start Arranging Your Transport