In this section
Truncus arteriosus
Provided by "Pediatric Heart Surgery — a reference for professionals"
Patient families can visit our truncus ateriosus page for more information and answers to common questions.
Pathophysiology
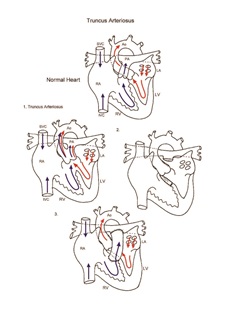
A persistent truncus arteriosus occurs when conotruncal septation fails to separate the truncal artery into a separate aorta and pulmonary artery during gestation. A single great vessel straddles a large outlet ventricular septal defect. This single great vessel gives rise to the pulmonary artery and ascending aorta. A spectrum of severity is based on the origin of the pulmonary arteries from the truncal artery. A main pulmonary artery may arise from the truncal artery (type I), the branch pulmonary arteries may arise separately but in close proximity (type II), or the branch pulmonary arteries may arise widely separate from the lateral aspects of the truncal artery (type III). Truncal valve abnormalities are often encountered in patients with this lesion. Truncus arteriosus results in unrestrictive left to right shunting of blood and pulmonary overcirculation. Congestive heart failure and pulmonary artery hypertension occurs. Pulmonary vascular obstructive disease will occur early if no intervention is undertaken. It is important to evaluate truncal valve function preoperatively, as significant stenosis or insufficiency of the truncal valve will require intervention at the time of surgery.
Surgical technique
Total repair of truncus arteriosus requires cardiopulmonary bypass and aortic cross-clamping. The pulmonary artery is separated from the truncal root, and the truncal vessel is closed directly or with a patch of synthetic material or cryopreserved homograft. A ventriculotomy is then made in the right ventricular outflow tract. The ventricular septal defect is closed, often using a running monofilament suture. Next, a valved homograft conduit is implanted, connecting the right ventricle to the pulmonary arteries. Truncal valve repair, replacement, or valvotomy is performed as an initial step when indicated. Truncal valve intervention adds significantly to the operation. Transesophageal echocardiography is performed to evaluate adequacy of repair. Cardiopulmonary bypass time and aortic cross-clamp time required are moderate. Delayed sternal closure is often required following repair of truncus arteriosus.
Postoperative considerations
Repair of truncus arteriosus is one of the more extensive cardiac procedures performed on neonates, especially when truncal valve repair or replacement is involved; the postoperative course is consequently more complex. Invasive monitors used include arterial and central venous catheters. An LA line is used when needed for hemodynamic management. LA pressure acts as a surrogate for left ventricular end diastolic pressure, an excellent indicator of left ventricular performance. Non-invasive monitors include NIRS (near infrared spectroscopy) probes to assess adequacy of regional and global perfusion and traditional pulse oximetry. Vasoactive agents might include epinephrine and/or milrinone. Numerous other agents are available and are tailored to the specific needs of the patient, targeting adequate oxygen delivery to the tissues of the body and optimization of cardiac output. Inhaled nitric oxide has proven useful in the management of postoperative pulmonary artery hypertension.
Bleeding is a potential postoperative complication. Suture lines exposed to systemic pressure and homograft suture lines under elevated pressure predispose these patients to early postoperative bleeding. Hemodynamic instability can occur following surgery, especially in patients who have truncal valve dysfunction. Atrioventricular conduction disturbances may be encountered, as surgical manipulation in the area of the atrioventricular conduction tissue is required for repair. Pacing capability should be readily available. Systemic arterial oxygen saturation following surgery should be normal. Intracardiac pressures should be normal. Length of hospital stay required following repair of truncus arteriosus is variable, but 10 days to 2 weeks is average.
Physician consultation line
Staffed 24 hours a day.
- Refer a patient
- Discuss a case
- Arrange a transport
- Direct admission
(414) 266-2460
Toll-free: (800) 266-0366
Make a referral
Find helpful forms and phone numbers for making a referral to a specialty clinic at Children's Wisconsin.
Arrange a transport
A physician-led, clinical team is available 24 hours a day for transports to Children's from across the country.
Start Arranging Your Transport