
Tucked away inside Children’s Wisconsin, winding through bustling hospital hallways, sits an auditorium where pediatric cardiac care leaders from all over the world convened for the third annual Herma Heart Institute Heart Summit. From October 3-5, some of the brightest minds in medicine traveled to this one-of-a-kind conference where expert insight met cutting edge technology for a truly remarkable three days.
And if that weren’t enough, the experience featured a live feed of Herma Heart Institute pediatric cardiologists performing cardiac catheterizations, along with a real-time open-heart surgery seen in stunning 3D video.
 “This is a unique conference,” said Peter Frommelt, MD, a pediatric cardiologist at the Herma Heart Institute who co-emceed the event. “Nobody is structuring educational medical conferences to include live, 3D imaging of congenital heart disease surgery and cardiac catheterization. This isn’t happening anywhere else. And I think that makes this a very special learning opportunity for the pediatric cardiology community.”
“This is a unique conference,” said Peter Frommelt, MD, a pediatric cardiologist at the Herma Heart Institute who co-emceed the event. “Nobody is structuring educational medical conferences to include live, 3D imaging of congenital heart disease surgery and cardiac catheterization. This isn’t happening anywhere else. And I think that makes this a very special learning opportunity for the pediatric cardiology community.”
Frommelt added that the event is now at the point where it has developed a reputation as a unique, innovative conference, and interest is growing with attendees from across the globe.
Focusing on one particular congenital heart disease condition helps set it apart, said Shakeel Qureshi, MD, of Evelina London Children’s Wisconsin, who also co-emceed the event. Starting with one particular heart defect and then expanding on it helps brings a greater level of understanding of a complex issue facing pediatric cardiologists and surgeons.
This year’s event focused on the failing Fontan, a complication of a special heart surgery that is challenging the pediatric cardiology community. Renowned experts from the United States and Europe formed the elite teaching panel that came to the Heart Summit to share their knowledge and experiences, discuss new techniques and novel approaches and then return home to bring that elevated level of care to their patients.
As the management of pediatric congenital heart defects continues to evolve, the Herma Heart Institute is committed to leading the way in innovative therapies. This is especially important as survival rates for even the most complex heart lesions continue to improve dramatically, leading to new and unforeseen long-term complications. The Herma Heart Institute is at the forefront of continued advancements to improve the quality of life for all survivors of congenital heart disease.
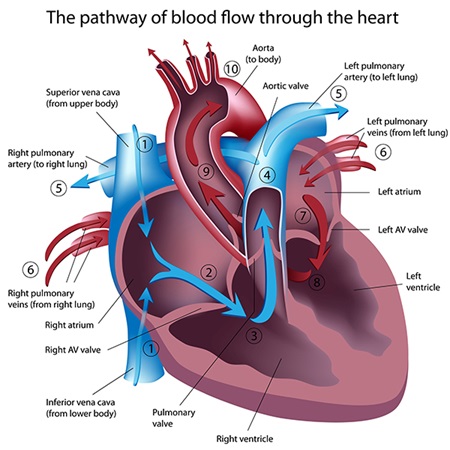 The human heart has four chambers: two upper atriums and two lower ventricles. The right atrium receives deoxygenated (blue) blood from the body, passes it to the right ventricle that pumps it through the pulmonary artery to the lungs where it becomes enriched with oxygen. The left atrium receives this oxygenated (red) blood from the lungs, passes it to the left ventricle where it is pumped to the aorta and throughout the body. The blue blood then returns to the right atrium and the cycle continues. Essentially, the atriums receive blood and then the ventricles pump blood.
The human heart has four chambers: two upper atriums and two lower ventricles. The right atrium receives deoxygenated (blue) blood from the body, passes it to the right ventricle that pumps it through the pulmonary artery to the lungs where it becomes enriched with oxygen. The left atrium receives this oxygenated (red) blood from the lungs, passes it to the left ventricle where it is pumped to the aorta and throughout the body. The blue blood then returns to the right atrium and the cycle continues. Essentially, the atriums receive blood and then the ventricles pump blood.
The Fontan procedure is a surgical operation designed to deal with one of the most difficult forms of congenital heart disease, the “functionally univentricular heart,” as described by Robert Anderson, MD, PhD, Institute of Child Health at University College London and one of the event’s keynote speakers. A child needing this procedure is born with only one functioning ventricle instead of two. Essentially, these children are born with half of a heart and will require an extensive remodeling of the heart to create separate circulations for the lungs and body.
The Fontan procedure accomplishes that separation and is usually successfully performed between the ages of 18 months and 3 years. While this procedure helps alleviate the immediate issues of the heart defect, it does not serve as the final fix. Patients frequently develop complications later in life, often in their teenage years. Those complications are referred to as “Fontan failure,” usually because that single functional ventricle gradually weakens and can no longer provide adequate blood flow to the lungs and the body.
While the failing Fontan served as that starting-point focus of the Heart Summit, the expert panels focused on the many ways in which the failure impacts children. A congenital heart defect has many long-term complications that need to be addressed, from the medical complications that can arise with the heart and other organs, to the social challenges that result from limited physical activity to the psychological stress and anxiety of experiencing multiple — often significant — medical procedures.
Jack Rychik, MD, Children’s Wisconsin of Philadelphia, in his lecture on “The Fontan Conundrum,” said, “Children needing a Fontan surgery are farther from a ‘cure’ than any other form of congenital heart disease.”
Not only is the condition challenging in its own right, the procedure — connecting the large vein that carries blue blood back from the body directly to the pulmonary artery so that blood flows to the lungs while bypassing the single ventricle — creates consequences of its own. One of those is excessive swelling and a build-up of scar tissue on the liver, which develops in all Fontan patients. Dr. Rychik noted there are a host of other physical and mental health concerns that these pediatric cardiologists must monitor.
“This is a very important topic in the field currently,” said Dr. Frommelt. “We have many babies born with a univentricular heart — one pumping chamber. And we’ve gotten very good at surgically making the blood go where it’s supposed to go. But there are many complications to not having two pumping chambers, so how do we manage that?”
This year’s Heart Summit helped address that question, and also demonstrated approaches in dealing with this problem by providing actual cases being performed that day in the Herma Heart Institute catheterization lab and operating room at Children’s Wisconsin.
 The live 3D heart surgery performed by Viktor Hraska, MD, PhD, surgical director of the Herma Heart Institute, was, of course, one of the highlights of the three-day event. Hraska began the morning by opening the Heart Summit, left to perform the surgery, and returned to the auditorium to discuss the operation before the end of the day. And all throughout, the live video feed to the operating room allowed Dr. Hraska and his team to discuss every step of the case with fellow experts and attendees. Importantly, the video feed allowed the complicated procedure to be viewed by all in attendance in a dazzling 3D broadcast.
The live 3D heart surgery performed by Viktor Hraska, MD, PhD, surgical director of the Herma Heart Institute, was, of course, one of the highlights of the three-day event. Hraska began the morning by opening the Heart Summit, left to perform the surgery, and returned to the auditorium to discuss the operation before the end of the day. And all throughout, the live video feed to the operating room allowed Dr. Hraska and his team to discuss every step of the case with fellow experts and attendees. Importantly, the video feed allowed the complicated procedure to be viewed by all in attendance in a dazzling 3D broadcast.
The visual experience was breathtaking. The ultra-high quality picture allowed viewers to see every detail involved in this complex procedure. And the 3D glasses gave an element of depth to the viewing experience that mimicked exactly what the surgeon was seeing.
“The surgical case was very complicated,” said Dr. Qureshi. “A brilliant job, a brilliant demonstration of the actual operating technique. But very important for us were the 3D pictures, so we were able to see into the heart in the operating room. It gives you the feeling of being there with the surgeon, seeing things from very close, and that’s the sort of experience that you’re not going to have at other conferences. It’s not easy to provide that degree of perspective to the audience.”
This surgery was performed on a 10-year-old girl who was born with one functioning ventricle. She underwent two open-heart surgeries as an infant — the first shortly after birth and another around 3 months old. As is commonly the case with single ventricle patients, her oxygen levels progressively decreased and she was now in need of a Fontan procedure. While most kids will undergo a Fontan between 1-3 years of age, complicating matters for this patient was a problem in her left lung that became apparent when she was 6 months old. For that reason, she was only now undergoing a Fontan.
 A common long-term challenge for patients who undergo a Fontan procedure is a condition known as “lymphatic congestion.” The lymphatic system is responsible for carrying important infection-fighting fluids throughout the body as well as removing toxins and waste. After a Fontan procedure, lymphatic fluid production increases and the body cannot keep up with the added pressure. When the lymphatic system becomes congested and backs up, toxins can build up and patients may develop a number of potentially life-threatening conditions.
A common long-term challenge for patients who undergo a Fontan procedure is a condition known as “lymphatic congestion.” The lymphatic system is responsible for carrying important infection-fighting fluids throughout the body as well as removing toxins and waste. After a Fontan procedure, lymphatic fluid production increases and the body cannot keep up with the added pressure. When the lymphatic system becomes congested and backs up, toxins can build up and patients may develop a number of potentially life-threatening conditions.
The question becomes: how do you perform a Fontan while allowing for proper drainage of the additional lymphatic fluid? The procedure performed by Dr. Hraska used a special technique that is truly cutting edge.
“Most pediatric cardiology centers are very excited about this surgical innovation,” said Dr. Frommelt, “but it is so new that most have not even done it yet.”
Dr. Hraska constructed a “bypass pathway for lymphatic drainage,” so that the lymphatics can now drain more easily back to the heart. This special surgical pathway involves connecting a large vein in the chest to the atrium that decompresses the lymphatic system. This operation can be done at the same time as the rest of Fontan procedure.
“There’s certainly been a handful of those surgeries done at different places, but only at elite centers,” said Dr. Frommelt. “We probably have the greatest experience doing that procedure, as it is an idea conceived by Dr. Hraska. The fact that we were able to demonstrate the procedure live to people coming to the Heart Summit is really just amazing.”
Seeing this done in 3D had a profound impact on attendees, added Dr. Frommelt.
“One of the expert panelists said that watching the real-time intraoperative 3D video actually gave him chills,” he said. “Despite having more than 25 years of experience working in the field, he had never been able to visualize what happens in the operating room quite like that.”
 Another developing aspect of caring for Fontan and other congenital heart disease survivors is how the diagnosis of heart disease impacts exercise and physical fitness. Understanding limitations posed by these conditions is important, but doesn’t necessarily mean these patients should avoid physical activity entirely.
Another developing aspect of caring for Fontan and other congenital heart disease survivors is how the diagnosis of heart disease impacts exercise and physical fitness. Understanding limitations posed by these conditions is important, but doesn’t necessarily mean these patients should avoid physical activity entirely.
To that end, doctors at the Herma Heart Institute have been developing a program called “Steppin’ It Up,” which encourages exercise and regular physical activity for these young survivors.
Joshua Kovach, MD, is a pediatric cardiologist at the Herma Heart Institute who leads the program and lectured on its latest developments at the Heart Summit. He said traditionally there has been more of a focus on limitations, on specifically figuring out exactly what level of activity is safe for these patients. But lately, there’s been a big push within the field to encourage more activity.
“Most families and most survivors are concerned about pushing the heart too hard,” Dr. Kovach said. “And what we find is that in most instances, congenital heart patients naturally limit themselves during activity so they never put themselves in that danger.”
While this may not mean that these patients should be pushing themselves to the point of an athlete competing at the highest levels, it can mean that more common physical activities — playing sports with friends, joining a rec league, etc. — should be encouraged, not avoided.
Studies from the program’s initial patient experiences showed significant physical improvement among participants, Kovach explained in his lecture. The study tested endurance by having participants do a shuttle run. For patients, that was their first time running — ever. The study’s findings, that exercise is safe and effective in improving activity performance, were so positive that they have received national attention at American Academy of Pediatrics and American Heart Association meetings.
Becoming more physically active can have a positive effect on many aspects of a patient’s overall health. As more and more young people are surviving these diseases during childhood, it’s becoming more apparent that fitness can impact their long-term health, their heart and lung function and their mental health.
“The feedback we’ve gotten most consistently from families is that their child seems to be more sure of themselves. They have more confidence,” said Dr. Kovach. “They don’t identify themselves as much as a ‘heart kid,’ but as somebody who is able to do things that other people can do. They no longer feel like they have to hold themselves back.”
Seeing this positive change in their children has benefited the parents, too. Watching their children participate in exercise can help quell anxiety over increased physical activity.
The “Steppin’ It Up” program began several years ago with just single ventricle patients who had undergone a Fontan procedure, and it has since expanded to other pediatric congenital heart diagnoses. The long-term goals are to extend the program from children to adult congenital heart disease survivors, and to find ways to target specific exercise concerns that families have.
 The third day of the conference focused on isomerism and heterotaxy syndrome — or, as Dr. Anderson put it in his lecture, “jumbled-up organs.” Basically, the body’s organs (heart, lungs, stomach, liver, spleen) aren’t where they should be.
The third day of the conference focused on isomerism and heterotaxy syndrome — or, as Dr. Anderson put it in his lecture, “jumbled-up organs.” Basically, the body’s organs (heart, lungs, stomach, liver, spleen) aren’t where they should be.
Isomerism appears in patients in a variety of different ways — and often with important and sometimes complex congenital heart defects. And with each unique patient brings a unique case of isomerism.
“There is no universal isomerism,” said Dr. Anderson.
However it manifests, isomerism is a real problem for patients. As Rohit Loomba, MD, of Advocate Children’s Wisconsin in Illinois, explained in his lecture on “Extracardiac Manifestations of Isomerism,” individuals with isomerism have only a 50 percent chance of surviving into their 30s.
As part of the conference, Dr. Anderson’s lecture included an in-depth look at four hearts brought from the Farouk Idriss Archives at the Anne and Robert H. Lurie Children’s Wisconsin in Chicago. Each heart displayed some type of isomerism. The close-up views provided by the high-definition display, broadcast on the auditorium’s 18-foot screen, showed in detail just how isomerism can appear in the heart, and how the condition can be detected.
The day also included lectures from geneticists to pulmonologists to pediatric cardiologists, making it a truly multidisciplinary discussion of a very complicated issue.
Throughout the three days, each lecture concluded with discussion, and despite the seriousness of the topics, the experts and emcees were able to approach it with a sense of humor, even bringing laughter into the auditorium.
“You can make education fun,” said Dr. Qureshi. “With humor, it relaxes people and they’re able to ask questions they might be reluctant to ask. And we’re hopefully able to answer them.”
A few laughs may have lightened the mood at times, but the conditions these experts are aiming to solve are as serious as it gets. The brainpower of the world’s leading experts brought together to educate and discuss just how to deal with these serious challenges inspired awe from those involved.
“There is so much interest, research, clinically innovative techniques occurring, and we were able to bring many experts from around the world together to give the most cutting edge snapshot of where we are now,” said Dr. Qureshi. “I think that’s remarkable.”

Pediatric services to include primary care, integrated behavioral health, child and family counseling and multiple specialty therapies.

Children and teens ages 5-18 can access mental health care immediately, with no appointment, referral or previous history with Children’s Wisconsin required.

The new Ashwaubenon Clinic is more than just a new building — it’s a resource designed with your child’s health in mind.

Medicaid provides the foundation for children’s health care in Wisconsin.

This can’t-miss event combines fun, fitness and fundraising to support kids in our community.

As part of our Connected for Kids partnership, Children's Wisconsin is increasing surgical care in Northeast Wisconsin.

Children’s Wisconsin and UW Health Kids are announcing a new joint venture for shared pediatric cardiac and adult congenital heart care services.
