It was Feb. 10, 2019, and a massive snowstorm engulfed most of Wisconsin. Rachel Berg was at her home in Shawano, 22 weeks pregnant with her second child.
She had just returned home from taking her daughter to Disney on Ice when she realized she had vaginal bleeding. Panicked, Rachel and her husband, Dylan, jumped in their car and headed to the emergency department at their local hospital. Once there, doctors discovered Rachel’s water had broken and she was already dilated. Knowing delivery could be imminent, doctors in Shawano wanted Rachel at the nearest hospital with a NICU.
Rachel and Dylan headed back out into the snowstorm, this time with Rachel in an ambulance and Dylan driving behind battling the blistering snow the entire 40-mile drive to Green Bay where Rachel was admitted and immediately put on strict bed rest.
Unbeknownst to her, Rachel had a pregnancy complication called preterm premature rupture of membranes (PPROM) that caused her water to break far too early. A week later when Rachel started having contractions, doctors were unable to stop them.
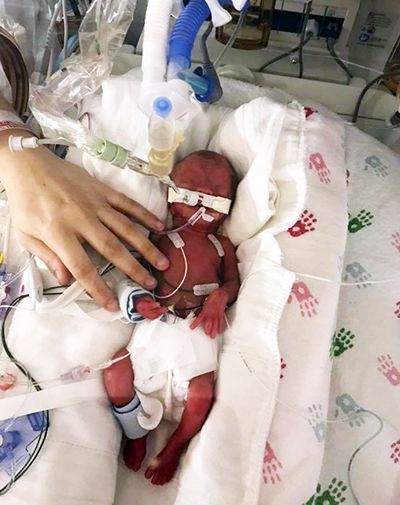 On Feb. 18, 2019, nearly four months early, Maddux was born. He weighed only 1 pound, 11 ounces.
On Feb. 18, 2019, nearly four months early, Maddux was born. He weighed only 1 pound, 11 ounces.
Maddux immediately had a breathing tube placed, and when he was 1 week old, he developed a serious infection in his intestines (known as necrotizing enterocolitis). He was then transferred to Children’s Wisconsin Hospital-Milwaukee.
Since the lungs are one of the last things to develop, it’s common for premature babies to need a breathing tube (known as a tracheostomy, or trach) and a ventilator (vent) to help them breath and take stress off the lungs. But as Maddux got closer to his due date age, Children’s Wisconsin doctors discovered he also had tracheomalacia, a rare condition where the cartilage of the trachea is weak and floppy. Every time doctors tried to remove his breathing tube, his trachea would collapse and block his airway. Doctors placed a tracheostomy — a breathing tube inserted through a hole in his neck that is attached to a ventilator — which allowed baby Maddux to breathe and eventually go home.
Every year, the Children’s Wisconsin Pulmonary Team cares for about 200 children with tracheostomies. A trach is needed when there is an anatomical issue or underdeveloped lungs due to prematurity. The ultimate goal is for kids to be on a trach for as short a period of time as possible and successfully transition off, a process called decannulation. Patients with a trach/vent normally meet with a multi-disciplinary team of providers in person every three to six months to assess their progress and take steps to wean them.
Thankfully for Maddux, tracheomalacia is a condition that resolves with age. Eventually, the floppy trachea tissue turns to cartilage and hardens. In spring 2020, just as the COVID-19 pandemic was starting to affect the United States, and businesses and schools were closing, Maddux was getting into mischief and starting to pull off the tubing attached to the trach in his neck that connected to his ventilator.
“Maddux was ripping his tubing off 100 times a day,” said Rachel. “I couldn’t even go to the bathroom or leave him for a second without him ripping his tubing off.”
An opportunity to innovate
 Due to the pandemic, Children’s Wisconsin — like hospitals all over the country — made the decision to postpone many non-time-sensitive appointments and procedures. But the trach/vent team knew their patients still needed to be seen, so they saw the pandemic as an opportunity to innovate their care model and implement virtual appointments to help keep their medically-compromised patients safe.
Due to the pandemic, Children’s Wisconsin — like hospitals all over the country — made the decision to postpone many non-time-sensitive appointments and procedures. But the trach/vent team knew their patients still needed to be seen, so they saw the pandemic as an opportunity to innovate their care model and implement virtual appointments to help keep their medically-compromised patients safe.
The Trach/Vent team partnered with the Children’s Wisconsin Digital Health & Experience (DHX) team to help bring this plan to reality. DHX was first established in 2017, initially to build technology that helped patients and families connect with their care team outside of an in-person visit through things like the patient portal, mobile apps and MyChart. In the fall of 2019, DHX launched a pilot program for video visits with surgical patients. When the pandemic hit, the DHX team moved quickly to scale video appointments to all departments.
"With COVID-19, video visits became an essential part of patient care, allowing patients to be seen when in-person appointments were not available," said Kimberly Cronsell, MD, medical director for Digital Health & Experience and associate chief medical officer at Children’s Wisconsin. “Eighteen months later, we are seeing the real impact on clinical outcomes that our teams have achieved by embracing this technology and actually changing the model they use to care for patients.”
The trach/vent team was already using software that allowed doctors and respiratory therapists to monitor various ventilator parameters remotely and review historical trends to see how patients were responding over time. Combined with virtual visits, providers were able to assess patients on camera, review their data and make vent adjustments in real time. Patients were still able to meet with all their normal specialists, with providers from respiratory, pulmonology, ENT and speech therapy swapping on and off the virtual appointment.
Rachel consulted with Julie Noe, MD, a pediatric pulmonologist at Children’s Wisconsin, about Maddux’s shenanigans. Dr. Noe told her Maddux’s behavior was his way of indicating that he didn’t need the ventilator anymore.
“We were able to set up a virtual appointment with Dr. Noe who watched Maddux breathe with his shirt off and watched his numbers and pulse ox remotely,” said Rachel. “Dr. Noe told us to follow Maddux’s lead and start weaning him from the ventilator.”
Vent weaning is a slow process. At first, Maddux would be off the vent for five minutes every 30-60 minutes. Gradually, Maddux built up his tolerance for being off the vent, and by Halloween 2020, he was fully weaned.
A novel use of technology
 Rachel and the Children’s Wisconsin team continued to let Maddux take the lead, and when he began taking his actual trach out of his neck, Dr. Noe told Rachel, “He’s telling us he’s done with it.”
Rachel and the Children’s Wisconsin team continued to let Maddux take the lead, and when he began taking his actual trach out of his neck, Dr. Noe told Rachel, “He’s telling us he’s done with it.”
The next step for Maddux was to trial capping his trach. A capping trial is used to test the ability to breathe completely through the nose and mouth. Normally this is done in-person with a speech therapist, but since Maddux lives 2.5 hours away from Children’s Wisconsin Hospital-Milwaukee, and since the care team had been in such close contact with Rachel via virtual visits, the therapist was able to mail the pieces to Rachel and she put the cap on during a virtual visit.
Completing these steps at home via virtual visits allowed Maddux to stay home and healthy, and progress seamlessly. Maddux was decannulated in May 2021, about three months faster than doctors originally expected.
Maddux wasn’t alone. Many kids in the trach/vent program showed better-than-expected results while utilizing virtual visits. Children’s Wisconsin decannulated 15 patients in 2018 and 17 in 2019. In 2020, the trach/vent team decannulated 28 patients. Even as the trach/vent team has moved back to in-person visits, virtual appointments continue to be part of their care model.
"The virtual visits were a novel way to use technology. People were hesitant before the pandemic, but we got better outcomes than we expected,” said Dr. Cronsell. “A lot of providers and staff realized it was a high-quality way to provide care.”
One reason for these incredible results is that the trach/vent team’s virtual appointments allowed providers to meet with patients more frequently, which helped them progress faster.
“The respiratory therapists were able to interface with patients more often than every three months, so if they were ready for a wean in the interim, we were able to move them forward as soon as they were ready,” said Jennifer Henningfeld, MD, pediatric pulmonologist and associate director of the Home Ventilator Program at Children’s Wisconsin.
The virtual appointments also offered greater convenience and peace of mind to families of kids who are on ventilators.
“Imagine a young baby coming to clinic and all of the things Mom or Dad would pack for that appointment,” said Dr. Henningfeld. “Now imagine that baby has a ventilator that is literally breathing for them and responsible for keeping them alive. You have to make sure the batteries are charged on the vent, plus bring a suction machine and other equipment in case of emergency. The technical complexity of bringing all of that equipment to help keep your baby alive is huge.”
Rachel agreed the virtual appointments were a huge timesaver.
“Making the trip down with all of the equipment took a lot out of everyone,” said Rachel. “We would leave at 5 a.m. and not get back until 7 or 8 p.m. and every time we would need to make arrangements for someone to care for our older daughter while we were gone. Plus with COVID-19, we wanted to reduce our exposure. The virtual visits would take 15-20 minutes as opposed to all of the pre-travel planning and an entire day away from home.”
From the start of COVID-19 until Maddux had his trach removed, Rachel estimates they had at least 10 virtual visits with different specialties, saving at least 3-4 trips to Milwaukee.
“I was very grateful for the virtual visits. Children’s Wisconsin knows our kids are high risk and they innovated to reduce exposure,” said Rachel. “Saving those trips saved our sanity a bit, too.”







