Congenital pulmonary airway malformation (CPAM) is a rare congenital birth defect that includes a cystic mass of abnormal lung tissue. A cystic mass is a noncancerous tumor that is filled with fluid or other material. This condition used to be referred to as congenital cystic adenomatoid malformation, or CCAM. In CPAM, the cystic mass does not function as normal lung tissue. Males have this condition slightly more often than females.
Congenital Pulmonary Airway Malformation
The Fetal Concerns Center at Children's Wisconsin diagnoses and treats congenital pulmonary airway malformations.
What Is Congenital Pulmonary Airway Malformation?
Where Does CPAM Occur?
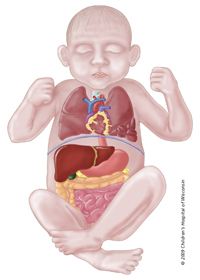
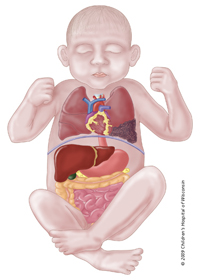
In most cases, CPAM is in only one of the lungs. (Less than 2% are in both lungs.) In 80-95% of cases, it is only present in one lobe of the affected lung. The right lung has three lobes, and the left lung has two lobes. CPAM can affect any of these lobes.
What Causes CPAM?
We do not know what causes CPAM. We do know that it is not related to anything the mother did or did not do during pregnancy. There are rare genetic associations, but a CPAM generally occur in otherwise healthy babies.
Types of CPAM
CPAM is classified into three types:
Macrocystic: Account for 50% of the postnatal (after birth) cases. These are lesions that contain large cysts that can easily be identified on prenatal ultrasound. This type generally has a very favorable outcome.
Macrocystic, which occurs in 50% of CPAM cases.
Microcystic lesions account for 40% of the postnatal cases. This type consists of more numerous smaller cysts that appear as abnormal looking lung on prenatal ultrasound without the large cysts noted in the macrocystic type. Some lesions contain a combination of macro and microcystic components.
Ultimately, the prognosis of a CPAM depends on its size and how much it compresses the development and function of the adjacent normal lung and CPAM's compress the heart, it may affect how the heart pumps blood to the fetus' body and can cause something called hydrops. Hydrops is a condition that causes fluid to accumulate in other body parts and can serious affect the health of the fetus.
Prenatal Diagnosis of CPAM
With the use of prenatal ultrasound, doctors are detecting CPAM earlier in pregnancy. This diagnosis must be confirmed because there are other birth defects that may appear similar to CPAM on ultrasound. Microcystic CPAM will appear as a bright mass in the area of the chest where only lung tissue should be and macrocystic lesions appear as large cysts whereas normal lung should be. The heart may be out of position, depending on the size and location of this cystic mass.
Microcystic lesions include more numerous and smaller cysts Microcystic lesions occur in about 40% of CPAM cases.
Testing During Pregnancy
If your obstetrician suspects CPAM, they will likely refer you to a maternal-fetal medicine specialist (a doctor who handles high-risk pregnancies). The maternal-fetal medicine specialist will perform an ultrasound and potentially other diagnostic tests to confirm the diagnosis. Although not all patients need a special test call an MRI, ultrasound findings may suggest the need for more advance imaging that can help your doctor determine the best treatment and provide more information about prognosis. Your doctor also may recommend a fetal echocardiogram. This is an ultrasound of the heart performed by a pediatric cardiologist. Doctors recommend it to rule out structural heart defects and to assess heart function.
The maternal-fetal medicine specialist will follow the growth of the mass by performing serial ultrasounds. That means you will have ultrasounds at regular intervals.
CPAM lesions may shrink in size; grow in size or remain the same size. If the CPAM grows, which will occur in a small number of cases, it can cause increasing problems for you and/or the baby, including the development of hydrops. Most lesions will either stay the same size or actually decrease in size or disappear as the pregnancy progresses.
Specialists You Will Work With
You also will meet with a variety of other specialists who will be caring for your baby after they are born. Which include:
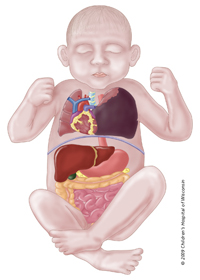
Large Micro or Macrocystic or a combination of the two lesions may cause other organs in the chest to shift.
- A neonatologist
- A pediatric surgeon
- A pediatric cardiologist (if a cardiac defect is confirmed or suspected)
How Does Congenital Pulmonary Airway Malformation (CPAM) Affect My Baby?
Many babies with CPAM will appear "normal" at birth without any apparent complications. If CPAM was not diagnosed prenatally, the baby would typically go home and either never be diagnosed or would be diagnosed later after a chest X-ray or after recurrent respiratory infections.
At birth, some babies born with CPAM will not be able to breathe effectively due to the large mass in their chest. If babies are unable to breathe effectively on their own, it can have an effect on their heart function. These babies need immediate intensive care to stabilize them until they can have surgery. Prenatal assessment generally allows us to identify those infants who may be a greatest risk of problems after birth.
In rare cases, "cysts" that are originally seen on the prenatal ultrasound may "disappear" on subsequent studies. Your surgeon may recommend a CT scan be performed after a few months of age to determine of the cyst completely resolved.
Does My Baby Need a Special Hospital?
Because of the possible need for immediate interventions in the delivery room, it is best if your baby is born at a hospital that can care for both you and your baby. This keeps the two of you together and avoids the trauma of having to transport your baby after birth. However, this need will be assessed during the pre-natal place of care an ultimately depends on an number of individualized factors.
Prenatal Surgery Options
There are a few indications for interventions before birth for babies with CPAM. The indication for such an intervention depends on the size of the lesion, whether it appears solid or cystic and the development of hydrops. If prenatal surgery is an option for your baby, your doctor will discuss it with you.
How Does CPAM Affect My Pregnancy?
If your obstetrician suspects CPAM, they will likely refer you to a maternal-fetal medicine specialist (a specialist who handles high-risk pregnancies) for a targeted ultrasound. The ultrasound will help confirm the diagnosis. Ultrasound also will help your doctor look at the general anatomy of your baby for associated anomalies, as well as to provide an idea of your baby's well-being.
Another diagnostic tool that is maybe useful in management of chest masses is an MRI. Fetal MRI is helpful in distinguishing a cystic type tumor from a solid one. Some affected fetuses will begin to accumulate fluid in various body cavities, such as in the lungs or abdomen, around the heart and under the skin. This is called hydrops. If this develops, it is an ominous sign, and may be an indication to deliver early or to examine the possibility for an in-utero operation or intervention to treat the lung mass before birth. These babies have a high-risk of dying in utero and of those who survive to be born, the majority will need significant medical and surgical support and are generally very ill.
How Do You Treat CPAM?
The traditional treatment of choice for CPAM is a lobectomy. This means that the lobe in the lung that contains the cyst(s) is completely removed. The timing of surgery depends on whether your infant has breathing problems or not. If there are no breathing problems, your baby will go home with you from the newborn nursery. They will need to return for surgery once they have been given time to grow. Your baby's surgeon will generally perform surgery at about 2 to 6 months of age. A chest X-ray and chest CT scan will be done as an outpatient procedure before surgery. Other factors may influence the appropriate timing of surgery.
If the mass is so large that it interferes with your baby's ability to breathe without help, we will perform surgery within the first week after birth. Before surgery, we will stabilize your baby and give they some time to adjust to life outside of your uterus, if possible. The doctor also will perform a general evaluation of your baby to check for any associated anomalies.
Some of the more severely affected infants may develop persistent pulmonary hypertension (PPHN). PPHN is a serious condition in which pressure in the lungs is high, forcing blood flow away from the lungs. This results in decreased levels of oxygen in the blood that goes to the body. High pressure in the lungs is normal for a fetus before birth because they are not using their lungs this way. However, after birth, this high pressure must decrease so that an adequate blood flow can pass through the lungs to rid the blood of carbon dioxide and pick up oxygen. Treatment for this condition may include inhaled nitric oxide or ECMO. ECMO stands for extracorporal membrane oxygenation. It is a machine that does work that the heart and lungs normally would do.
At birth, if the size of the CPAM requires immediate assistance, we will place a tube into your baby's airway to help them breathe. If possible, parents will be allowed to see and hold your baby in the delivery room. When it's necessary, your baby will be transferred to the Neonatal Intensive Care Unit (NICU) for treatment.
If your baby goes to the NICU and requires immediate care for breathing issues, we also may need to place some special lines. For example:
- The umbilical cord of a newborn typically contains two arteries and one vein. A flexible tube for giving intravenous solutions called an umbilical venous catheter will be placed in the vein in the umbilical cord so nourishment (vitamins, minerals, calories, fat) and medications can be given for a prolonged period of time.
- Another flexible tube will be placed in one of the arteries of the umbilical cord. This is called an umbilical artery catheter. We use this line to give IV fluid, remove blood for testing and monitor blood pressure.
Medications given before surgery could include:
- Narcotics to keep your baby free from pain
- Paralytics to keep your baby from moving
- Blood pressure medication to maintain an adequate blood pressure
What To Expect After Surgery
Treatment after surgery depends on a number of factors, including:
- When the surgery is done
- The size of the CPAM
- How much lung was removed
- If the CPAM involves both lungs or more than one lobe, your baby may have more limited breathing.
- General health of the baby. If your baby has hydrops, unfortunately, they will likely have a much rockier course with a poorer prognosis. Some babies with hydrops will not survive to have surgery.
Breathing tube: After surgery, your baby may need continued help to breathe effectively. We will keep the special tube (endotracheal tube) that had been placed during surgery into the windpipe. This tube helps with your baby's breathing, but it will also keep your baby from making sounds. It will be removed when the specialists feel your baby can breathe safely without the assistance of the tube.
Blood draws: They may need frequent blood draws for lab work to monitor oxygenation, electrolytes, blood count and other things.
Medications: After surgery, your baby may need a variety of medications including:
- Antibiotics to fight infection
- Pain medication to control pain after surgery
- Blood pressure medication to stabilize and maintain an adequate blood pressure
- Sedation to keep your baby quiet so they do not become agitated
- Paralytics to keep your baby from moving
IV lines: Your baby will have IV lines placed. The type of lines used will depend on the age at which the surgery is performed. If surgery is done soon after birth, the umbilical cord artery and vein will be used. Other IV lines can be placed in your baby's hands, arms, scalp, feet or lower legs. These are started just as they were for you while in labor.
Chest tube(s): Your baby also may have a chest tube on the side of the chest where the CPAM was removed. This helps the lung on that side re-expand into the chest space where the mass used to be. It will also drain any fluids that accumulate in the chest.
Urinary catheter: Your baby may have a urinary catheter passed into his or her bladder that was placed during surgery. This helps us keep an accurate assessment of how much urine the kidneys are making and allows us to test the urine to ensure your baby's well-being. It is temporary and usually removed soon after surgery.
IV nourishment: Your baby will not be able to eat until his or her condition has stabilized, but we will continue to give nourishment with IV fluids. Because babies with CPAM may not eat for a while, special nourishment is given through the veins, typically through a central line or UVC. Total parenteral nutrition is an IV solution that contains protein, fats, sugar, vitamins and minerals. This will supply your baby with all his or her nutritional requirements until they are able to take food by mouth.
Will I Be Able To Help Care for My Baby After Surgery?
Yes. Ask your baby's nurse about ways to interact with and care for your baby.
If you had planned to breastfeed your baby, you can start pumping your breasts and freezing the breast milk while you are still in the hospital. A lactation consultant can answer your questions. Your milk will be frozen and stored in the NICU until your baby is ready for it. The NICU has breast pumps and private rooms available to you when you are visiting.
When Can My Baby Go Home?
Your baby will go home when they can eat enough to maintain and gain weight and can breathe well without help. The length of stay for a baby with CPAM varies depending on the severity of his or her condition and his or her response to treatment.
If the cyst(s) is large, involves more than one lobe, or is bilateral (involves both lungs) and requires immediate intervention and surgery, the stay will likely be longer. The average stay for this course of care can range from 4 to 12 weeks.
This is compared to a baby who has milder symptoms or is able to wait 2 to 6 months for surgery. Their average stay can range from a few days in the newborn nursery to 1 or 2 weeks in the NICU. If there are associated anomalies (more common with type II CPAM), it can prolong or complicate the length of stay as well, no matter how large or small the CPAM is.
What Is My Baby’s Long-Term Prognosis?
The long-term outcome for infants who have the cyst(s) removed is excellent. This is especially true when there are no other anomalies and hydrops is not present. After the cyst is removed, the lungs grow to compensate for the part that was removed. These children usually have no limitations on their activities and have no increased risk for respiratory complications. However, if the CPAM is not removed, there is an increased risk of it becoming cancerous and cause problematic lung infections.
Learn more about the Surgery Program at Children's Wisconsin.
Our Locations
Our Doctors




