In this section
Tracheal esophageal fistula and esophageal atresia
What is TEF/EA?
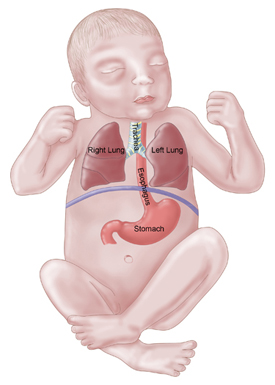
The trachea is the windpipe and goes to the lungs. The esophagus is the "food pipe" and goes to the stomach. They run side-by-side through the neck and upper chest. Normally the trachea and the esophagus are not connected in any way. Very early in the development of a fetus a single tube will divide to form the esophagus and the trachea. For an unknown reason, sometimes the wall does not form properly and a tracheal esophageal fistula and/or esophageal atresia may be the result.
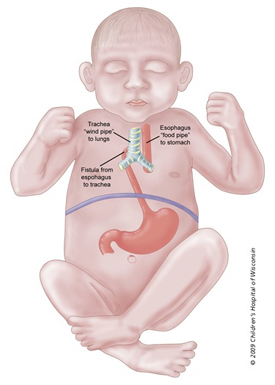
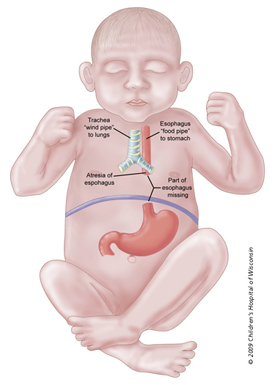
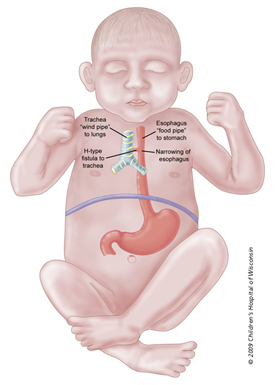
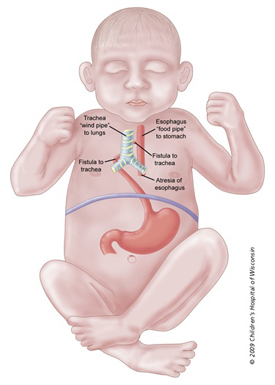
A fistula is an abnormal connection and atresia means a blockage. An esophageal atresia is a blockage in the esophagus, which can occur with or without a fistula. There are a variety of ways the esophagus and trachea can be connected with a fistula.
The five most common variations of a TEF are:- A middle section of the esophagus is missing and the windpipe is connected to the lower end of the esophagus with a fistula; this is the most common type and accounts for 86 percent of cases.
- An absence of a portion of the esophagus with no fistula to the trachea; neither end is connected to the windpipe; this is more rare accounting for 8 percent and is a true esophageal atresia (with no fistula).
- The esophagus is complete (but may have a portion that is too narrow) with a fistula to the trachea; this is an H-type and accounts for 4 percent of cases.
- A middle section of the esophagus is missing and there is a fistula to the trachea from the upper portion of the esophagus; This accounts for 1 percent of cases.
- An absence of a portion of the esophagus with fistula connections to the trachea from both the upper and lower portions of the esophagus; this accounts for 1 percent of cases.
TEF/EA is one of the most common gastrointestinal birth defects. It has a slightly higher incidence in males than females. The incidence rate of TEF/EA is approximately 1 in 4,000 live births. Of the babies born with TEF/EA, approximately 50 percent will have an associated birth defect. The most commonly associated birth defect is cardiac, seen in about 25 percent of these patients. Atrial and ventricular septal defects are the most common cardiac disorders seen. We do not know the cause of TEF/EA but it is thought to occur around the fourth week of pregnancy as the various systems are developing. We know it is not due to anything the mother did or did not do during pregnancy.
Occasionally there will be a clustering of birth defects along with the TEF/EA, but no genetic association has been found. The acronym VACTERL is used to describe this combination of birth defects. Each letter of the acronym stands for a type of anomaly:
- Vertebral anomalies
- Anus, imperforate
- Cardiac
- Tracheo-Esophageal fistula or atresia
- Renal anomalies
- Limb anomalies (radial dysplasia)
Prenatal Diagnosis of TEF/EA:
Sometimes a TEF/EA will be diagnosed or strongly suspected before birth through routine ultrasound. The inability to see a stomach and maternal polyhydramnios during an ultrasound are suspicious findings that may indicate TEF/EA. Normally, a baby in the womb will swallow and breathe in the amniotic fluid. If the fistula is so narrow or restrictied in flow that it does not allow for this, the amniotic fluid will build up. This excessive amount of amniotic fluid is called polyhydramnios. No stomach is seen because the baby is not swallowing amniotic fluid and the stomach is empty. If there is a large fistula however, a stomach bubble might be seen and the diagnosis may be missed.
A more accurate means to diagnose a TEF/EA is to see an enlarged proximal or upper pouch. With this picture, the esophageal closure is seen and a more definitive diagnosis is made.
Your obstetrician will likely refer you to a specialist that handles high-risk pregnancies. These doctors are called perinatologists. With either of the above findings, a targeted ultrasound is needed to look at all of the baby's systems because of the high incidence of associated anomalies.
How does TEF/EA affect my baby?
The affects that TEF/EA will have on your baby depends on the type of TEF. If there is a closure in the upper esophagus, the baby will not be able to swallow saliva or food. The baby will have fine, frothy bubbles in the mouth and sometimes coming out the nose. Any attempt at feeding will result in choking, coughing and the formula will come back out because it has no place to go. If the infant aspirates (breaths foreign matter into the lungs), he or she may develop respiratory distress.
A fistula may increase the chances of respiratory problems. If the fistula is from the upper pouch or is the H-type, symptoms may only be seen when the baby eats. With a fistula of the upper pouch, when the baby eats there may be severe respiratory symptoms. The baby may become blue and appear to choke because the formula can pass through the fistula, into the trachea and then into the lungs. Occasionally, babies with the H-type may go home and return with pneumonia because the food has been going into the lungs as well as into the stomach. Pneumonitis (inflammation of the lungs) and atelectasis (collapse of part of one or both lungs) can develop quickly in these babies. When the fistula is in the lower portion of the esophagus, there may be reflux (backward flow) from the esophagus, through the fistula, into the trachea and into the lungs. Abdominal distention may also be seen with a fistula connection from the lower pouch because the fistula allows air to enter the stomach and intestines.
As many as 50 to 70 percent of the babies with TEF/EA will have an associated anomaly. VACTERL is an acronym used to describe the more commonly associated combination of defects. Most babies will not have all of these associated defects but many will have at least one other defect.
After birth, the inability to pass a tube into the stomach is cause to suspect TEF/EA. A chest X-ray will be done to confirm the presence of a closure. Contrast enhanced studies are not normally necessary to confirm a diagnosis. However, a contrast study may be needed to identify and locate a fistula.
How does TEF/EA affect my pregnancy?
If your obstetrician suspects a problem with your baby, you will likely be referred to a perinatologist. These are doctors who handle high-risk pregnancies. The perinatologist will perform a targeted ultrasound to look for a fetal anatomy.
Prenatal diagnosis of EA/TEF is difficult. so your baby will need a thorough evaluation after birth to confirm the diagnosis. TEF/EA may be suspected if no stomach bubble is seen in the fetus and there is polyhydramnios. These two signs are cause for suspicion but are not conclusive for the diagnosis. Rarely, an enlarged upper esophageal pouch may be seen, which can help diagnose esophageal atresia. When TEF/EA is suspected before birth, it is recommended that chromosomes be evaluated as TEF/EA can be associated with Trisomy 21 (Down syndrome). This is done by amniocentesis. The risks and benefits of this procedure will be discussed with you before it is performed.
Because of the high incidence of cardiac disorders associated with TEF/EA, a fetal echocardiogram may also be recommended. Echocardiogram is an ultrasound that looks at the heart's anatomy, blood flow and circulation. A pediatric cardiologist will perform this test before birth and possibly again after birth to confirm the diagnosis.
Polyhydramnios can cause some issues with the pregnancy that will require follow-up. Because the uterus is larger than normal, preterm labor can sometimes become an issue. Premature birth is a complicating factor because the baby's size may determine when reparative surgery can be done. Active measures may be required to continue the pregnancy and stop preterm labor. These can range from bed rest at home to hospitalization with medication to stop contractions (tocolytics), to reduction amniocentesis. With reduction amniocentesis, amniotic fluid is removed using a hollow needle inserted through the mother's abdomen and uterine wall, with the guidance of ultrasound. Unfortunately reduction amniocentesis provides only temporary relief. The fluid will accumulate back to the original volume, usually within a week. Because of this, it is used primarily to help mothers who are having difficulty breathing because of the pressure of the uterus on the diaphragm. If a reduction amniocentesis is considered medically necessary and you have not previously had a genetic test, this may be discussed with you as a possibility at this time, as well.
How is TEF/EA treated?
Soon after delivery, a tube is passed into the esophagus to keep the pouch and/or fistula empty of secretions. The baby will be kept in an upright position to allow secretions to pool in the pouch and be suctioned out by the tube. The baby will be examined for any other birth defects. This examination can include a renal ultrasound (to look at kidneys), echocardiogram (to examine the heart), a chest X-ray and possibly X-rays of the limbs (especially arms). These tests will help determine if the baby has VACTERL syndrome.
The baby will be stabilized and the defect will be evaluated before surgery is attempted. Your baby will not be able to eat until some time after surgery. Special IV lines are put in place prior to surgery. These can include two small catheters in the baby's umbilical cord. The umbilical cord normally has two arteries and one vein. A catheter-type IV will be put into the one vein to provide nutrition.This is called an umbilical venous catheter. Because these babies do not eat for a period of time, special nourishment is given through this IV. Total parenteral nutrition is an IV solution that contains protein, fats, sugar, vitamins and minerals. This will supply your baby with all his/her nutritional requirements until he/she is able to take food by mouth. There are two components to TPN. One is a yellow IV solution that contains everything but the fats. The fats are in another solution that is white.
A second IV catheter will be placed in one of the arteries. This is called an umbilical artery catheter. Through this line, fluids and medications can be given, blood pressure can be monitored and blood can be removed for lab work. Your baby will require frequent blood draws for lab work to monitor oxygenation, electrolytes, blood count and other things. Another IV may also be place in the baby's hand, arm, scalp, lower leg or foot.
Your infant may be on a variety of medications, including antibiotics to fight infection, pain medication and beta blockers to help dry up the oral secretions.
Surgery will be done sometime in the first week. The repair may be primary, meaning the two ends of the esophagus are close enough that they can be reconnected. This is the typical procedure done with proximal blind pouch and lower esophageal fistula. With true esophageal atresia with no fistulas, some may be a primary repair while others will be staged repair. With a staged repair, the surgeon waits for the esophagus to grow before doing the final repair. When the ends are too far apart, the surgery is done in stages. During the first surgery, a gastrostomy tube (GTT) may be placed and the fistulas which are allowing foreign matter into the trachea may be removed. The GTT will provide a way to feed the baby until the final repair can be done. A GTT is a tube that is placed into the stomach through a small surgical incision in the abdominal wall. Formula or breast milk can be given through this tube directly into the stomach. There are a variety of surgical procedures that can be used if the pouches are too distant from one another. All attempts are made to use the baby's own esophagus because the esophagus includes a layer of muscle that helps move food to the stomach. The surgeon will discuss with you the procedure that is recommended for your baby.
What about after surgery?
After surgery, your baby may not be able to breathe effectively on his or her own. A special tube called an endotracheal tube, or ETT, will be placed at the time of surgery (if it was not needed earlier) to assist with breathing. The tube is passed through the vocal cords and into the windpipe. While this tube is in place, your baby will not make any sounds because of its position between the vocal cords. This tube will probably stay in for a time after surgery until the baby can breathe effectively on his or her own. Babies with a fistula have an area of "floppy" airway and an area that was repaired with surgery. These areas need time to heal well, so the ETT will need to stay in place longer.
Your baby may look swollen after surgery. This swelling is called edema and will go away as your baby gets stronger. The sutures needs time to heal before oral feedings are attempted. About 7 to 10 days after surgery, a contrast X-ray will be performed to confirm the success of the repair and ensure there are no leaks. No attempt at feeding by mouth will be done until this study confirms that everything is closed without leaks.
The head of the bed is kept at a 45-degree angle and the neck will be kept slightly flexed after surgery. The baby will continue to require frequent suctioning. Sometimes, even with a primary repair, a gastrostomy tube will be placed so that food can be given while sutures heal and the intestinal tract begins functioning again. Initially, the GTT may be placed to suction air and secretions out of the stomach and prevent reflux of the stomach contents near the sutures.
Will I be able to help care for my baby after surgery?
Yes. Please ask your baby's nurse about ways to interact with and care for your baby. If you had planned to breastfeed your baby, you can begin to pump your breast milk while you are still in the hospital. A lactation consultant can assist in answering your questions. Your milk will be frozen and stored in the Neonatal Intensive Care Unit (NICU) until your baby is ready for it. The NICU has breast pumps and private rooms available to you when you are visiting. You can bring in pictures, small toys, booties and blankets for your baby while he or she is in the NICU. The Fetal Concerns Center includes a tour of the NICU before your baby is born. This helps you get a better idea of where your baby will go after delivery and the facilities available to you as you learn to care for your baby while he or she is still in the hospital.
When can my baby go home?
Your baby will go home when he or she is eating and tolerating enough food to allow them to grow and gain weight. The amount of time your baby will be in the hospital will vary depending on their gestational age at the time of delivery, whether a primary or staged repair is needed, healing after surgery, ability to take in food and associated anomalies.
What is my baby's long-term prognosis?
The prognosis for survival for an isolated TEF/EA is excellent. An associated anomaly can alter that prognosis. The most significant causes of poor prognosis are complex cardiac anomaly and chromosomal abnormalities. Babies with repaired TEF/EA may have problems with swallowing due to altered muscular movement of food down the esophagus or due to narrowing of the esophagus after surgery. Sometimes, a narrowed esophagus can be widened with a surgical procedure. This procedure may need to be repeated more than one time in the child's lifetime. Your child may be referred to a therapist who can teach special techniques and exercises to help him or her swallow. Failure to thrive is a potential complication for these babies. Another common problem is gastrointestinal reflux disease. Approximately half of the children with TEF/EA will experience GERD. Special medicine can be prescribed to help treat this condition. Pulmonary complications such as bronchitis and frequent pneumonia are occasionally seen.
Learn more about services at Children's Wisconsin:
Get a second opinion
(414) 240-1831
Research and outcomes
Our outcomes reports help families and partner providers make the most informed healthcare decisions. Learn more about our surgical outcomes and current research studies.